
HSC Research Brief No. 8
October 2008
Judith H. Hibbard, Peter J. Cunningham
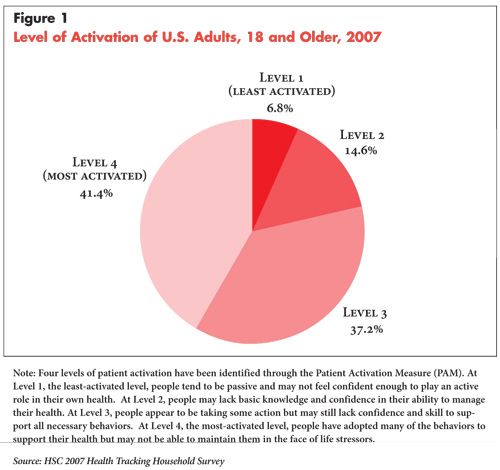
Patient activation refers to a person’s ability to manage their health and health care. Engaging or activating consumers has become a priority for employers, health plans and policy makers. The level of patient activation varies considerably in the U.S. population, with less than half of the adult population at the highest level of activation, according to a new study by the Center for Studying Health System Change (HSC) (see Figure 1). Activation levels are especially low for people with low incomes, less education, Medicaid enrollees, and people with poor self-reported health. Higher activation levels are associated with much lower levels of unmet need for medical care and greater support from health care providers for self-management of chronic conditions.
![]() here is a growing consensus that activating and engaging consumers is an essential component to health care reform in the United States. The health care choices of individual consumers and daily management of their own health can profoundly affect health care utilization, costs and outcomes. While there are sharp differences between advocates of a strong government role in health care reform and those who believe reform should be achieved primarily through the private sector, most health care reformers at least acknowledge that improvements in quality, cost containment and reductions in low-value care will not occur without more informed and engaged consumers and patients. Payment reform and structural changes to care delivery only address one side of the equation. The other side is consumers and patients becoming more informed decision-makers and managers of their health.
here is a growing consensus that activating and engaging consumers is an essential component to health care reform in the United States. The health care choices of individual consumers and daily management of their own health can profoundly affect health care utilization, costs and outcomes. While there are sharp differences between advocates of a strong government role in health care reform and those who believe reform should be achieved primarily through the private sector, most health care reformers at least acknowledge that improvements in quality, cost containment and reductions in low-value care will not occur without more informed and engaged consumers and patients. Payment reform and structural changes to care delivery only address one side of the equation. The other side is consumers and patients becoming more informed decision-makers and managers of their health.
From a policy perspective, this represents a serious challenge, with limited evidence and few strategies available to achieve this end. A first step is to understand what it means to be activated and engaged and the current extent of activation in the U.S. population. This Research Brief examines patient activation, how it varies by key socioeconomic characteristics, and how activation is related to other aspects of patients’ experiences with the health care system.
![]() ctivation refers to people’s ability and willingness to
take on the role of managing their health and health care. The Patient Activation
Measure (PAM) was designed to assess an individual’s knowledge, skill and confidence
in managing their health.1 The PAM consists of a 13-item
scale that asks people about their beliefs, knowledge and confidence for engaging
in a wide range of health behaviors (see Appendix). Based
on responses to the 13-item scale, each person is assigned an “activation score.”
ctivation refers to people’s ability and willingness to
take on the role of managing their health and health care. The Patient Activation
Measure (PAM) was designed to assess an individual’s knowledge, skill and confidence
in managing their health.1 The PAM consists of a 13-item
scale that asks people about their beliefs, knowledge and confidence for engaging
in a wide range of health behaviors (see Appendix). Based
on responses to the 13-item scale, each person is assigned an “activation score.”
The PAM has been shown to be a valid measure of activation. For example, individuals identified as highly activated according to the measure are more likely to obtain preventive care, such as health screenings and immunizations, and to exhibit other behaviors known to be beneficial to health. These include maintaining good diet and exercise practices; self-management behaviors, such as monitoring their condition and adherence to treatment protocols; and health information seeking behaviors, such as asking questions in the medical encounter and using quality information to select a provider.2
Most importantly, studies show that activation is changeable over time. One study showed that gains in activation over a six-month period were followed by improvements in several health-related behaviors.3 Another study showed that consumers who get support for being proactive about their health from their care team, from their coworkers and supervisors, and from friends and family tend to be more activated and to engage in healthier behaviors and choices.4
![]() rior research using the PAM has relied on relatively small
samples or groups, such as health plan enrollees, Medicaid enrollees in several
local areas, and older adults with chronic conditions. HSC’s 2007 Health Tracking
Household Survey is the first large nationally representative survey to include
the PAM to assess the level of activation in the U.S. population (see Data
Source).
rior research using the PAM has relied on relatively small
samples or groups, such as health plan enrollees, Medicaid enrollees in several
local areas, and older adults with chronic conditions. HSC’s 2007 Health Tracking
Household Survey is the first large nationally representative survey to include
the PAM to assess the level of activation in the U.S. population (see Data
Source).
Research on patient activation suggests that individuals go through phases or levels on their way to becoming effective self-managers. These levels are also useful for designing interventions to help people improve their ability to self-manage. Four levels of activation based on the individual’s overall activation score have been identified. At the first or lowest level, people tend to be passive and may not feel confident enough to play an active role in their own health. At the second level, people may lack basic knowledge and confidence in their ability to manage their health. At the third level, people appear to be taking some action but may still lack confidence and skill to support all necessary behaviors. At the fourth level, people have adopted many of the behaviors to support their health but may not be able to maintain them in the face of life stressors.
Less than half of all adults in the United States (41.4%) are in the highest level of activation, according to findings from HSC’s 2007 Health Tracking Household Survey. Even at this level, people still struggle to maintain healthy behaviors but tend to have the skills and confidence to manage their health in a more proactive way. On the other hand, relatively few people (21%) are in the lowest levels of activation (Levels 1 and 2), where basic skills and knowledge are lacking.5
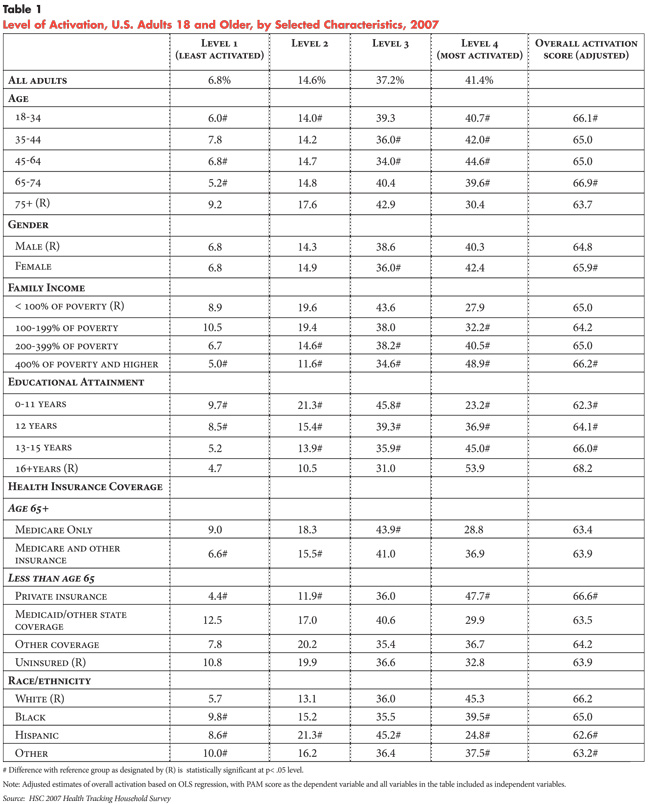
![]() here is a substantial amount of variation in activation
levels across the U.S. population. Those who are younger, more educated and
have higher incomes tend to be more activated (see Table 1).
Similarly, those with private health insurance tend to have higher activation
than those with Medicaid or those with only Medicare. Racial and ethnic differences
in activation are also apparent, with Hispanics having much lower activation
levels compared with other groups.
here is a substantial amount of variation in activation
levels across the U.S. population. Those who are younger, more educated and
have higher incomes tend to be more activated (see Table 1).
Similarly, those with private health insurance tend to have higher activation
than those with Medicaid or those with only Medicare. Racial and ethnic differences
in activation are also apparent, with Hispanics having much lower activation
levels compared with other groups.
Most of the differences in activation by education, race/ethnicity, age and insurance coverage remain after controlling for other characteristics. The one exception is that income differences narrow considerably after controlling for education, meaning that most of the income difference in activation reflects differences in educational attainment that are correlated with income.
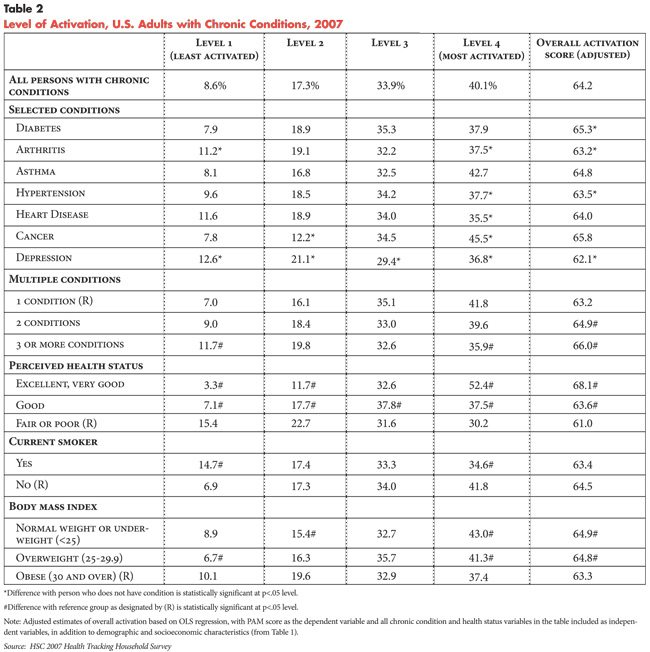
Activation also varies by the type and number of chronic conditions, as well as other measures of health status. Overall, people with chronic conditions are more likely to have lower levels of activation—about 26% in Level 1 or 2—compared with people without any chronic conditions—about 18% in Level 1 or 2 (findings not shown).
However, among people with chronic conditions, there are considerable differences by condition and other health characteristics. For example, people with depression tend to be the least activated, while those with cancer tend to have higher activation (see Table 2). People with multiple chronic conditions, who report their health as fair or poor and who are obese are less activated than people with a single condition or those with better health indicators.
However, the adjusted activation scores indicate that after accounting for differences in health status, obesity and other characteristics, people with multiple chronic conditions tend to have higher activation scores compared with those with only a single chronic condition. All other things being equal, having multiple conditions may necessitate greater self-management and more careful monitoring of one’s own health. Moreover, health care providers may be more proactive about teaching self-management skills to patients with multiple conditions.
To some extent, activation reflects the degree to which one feels “in charge” of one’s own health. People with more resources in the form of education and income score higher on the activation measure, while people who have experienced repeated failures in their ability to manage their health, such as those who are obese or who smoke, score lower.
It is important to note that it is difficult to discern the direction of causality in the observed relationships as the data were collected at a single moment in time. Longitudinal data are needed to determine whether poor health status causes lower activation, or whether low activation and passivity contribute to poorer health. Likely the causality operates in both directions, although low activation resulting from poor health may lead to a vicious cycle that precludes behaviors that could improve health.
Moreover, while there are significant associations between demographic and health status characteristics and activation levels, there is also considerable variation in activation within categories of education, income and health status. For example, while there is a strong correlation between education level and activation, 15 percent of college graduates are in the lowest two levels of activation, while 23 percent of those with less than a high school education are in the highest level of activation. This suggests both that lower educational attainment need not be a barrier to higher activation and that knowing the socioeconomic characteristics of a population is insufficient to identify their activation level.
![]() ltimately, the value of more highly activated patients
is that it will lead to better health outcomes and health practices. For example,
prior research has shown that higher levels of activation are associated with
higher levels of preventive health behaviors and preventive care, as well as
increased self-management of health conditions.6 Part of
being more activated is seeking and using relevant health information. For example,
those who are more activated are more likely to report that they read about
possible side effects when they get a new prescription drug. Ninety-four percent
of those at the highest level of activation read about possible side effects,
compared with 74 percent of the least activated (findings not shown).
ltimately, the value of more highly activated patients
is that it will lead to better health outcomes and health practices. For example,
prior research has shown that higher levels of activation are associated with
higher levels of preventive health behaviors and preventive care, as well as
increased self-management of health conditions.6 Part of
being more activated is seeking and using relevant health information. For example,
those who are more activated are more likely to report that they read about
possible side effects when they get a new prescription drug. Ninety-four percent
of those at the highest level of activation read about possible side effects,
compared with 74 percent of the least activated (findings not shown).
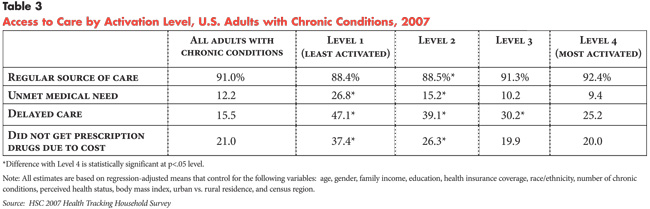
Crucial to positive health outcomes is the ability to obtain needed health care services. While health policy often focuses on the financial and health insurance coverage barriers to obtaining needed medical care, it is likely that more highly activated patients have greater success in navigating a highly complex and often confusing health care system. For example, people with chronic conditions who are at lower levels of activation are much more likely to report unmet medical needs, to delay care and to have unmet prescription drug needs (see Table 3). Less activated people are also somewhat less likely to have a usual source of care. These differences remain even after controlling for socioeconomic and health status and likely reflect the more passive approach that people at lower levels of activation often take in managing their health. These findings also may indicate that those who are less activated are more vulnerable to barriers to care and are more easily dissuaded from taking action when faced with financial or health system barriers.
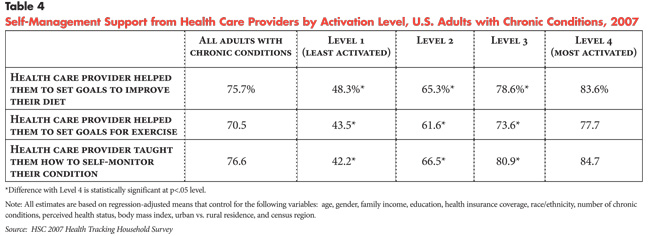
At the same time, people with chronic conditions who are more activated appear to get more support from their providers in managing their health. For example, 83.6 percent of those at the highest activation level reported that their health care provider helped them set goals to improve their diet, compared with 48.3 percent at the lowest activation level (see Table 4). Highly activated patients also were more likely to report that their provider helped them set goals for exercise and taught them how to self-monitor their condition. In sum, more activated patients appear to have more positive and supportive health care experiences. As the direction of causality is unclear, this may either reflect highly activated people being more adept at choosing more supportive health care providers that will give them the care they need, or that greater support from providers contributes to higher activation levels in patients.
![]() ctivated consumers take a proactive approach to managing their health and health care. Activation level is a reflection of the individual’s beliefs about their role in managing their health, as well as their knowledge and confidence for doing so.
ctivated consumers take a proactive approach to managing their health and health care. Activation level is a reflection of the individual’s beliefs about their role in managing their health, as well as their knowledge and confidence for doing so.
This is a much broader view of consumer activation than is often the focus of consumer-directed health plans, which primarily seek to increase consumer cost sensitivity. From a policy perspective, cost sensitivity by itself may be a necessary but not sufficient condition for greater consumer engagement. Indeed, increased cost sensitivity is but one manifestation of a more activated consumer, in which personal resourcefulness, education and motivation are necessary preconditions for seeking information on cost, quality and other important aspects of health care. A particularly striking finding is that higher activation levels are associated with much fewer problems with access to care, even when controlling for insurance coverage and income, which may reflect greater resourcefulness among more highly activated people in navigating the complexities of the health care system and overcoming barriers.
The findings indicate that activation levels differ considerably across socioeconomic and health status characteristics. Because activation levels are linked to important outcomes, such as seeking care, seeking information and health behaviors, and because it is a changeable attribute, it is a potentially important lever for change.
Other research indicates that people who live, get their health care and work in supportive environments that enable proactive health behaviors tend to be more activated.7 Although it is not possible to determine the direction of causality, one interpretation of the findings in this study is that support from physicians—teaching patients how to monitor or set up an exercise plan—stimulates patient activation. If this is correct, then encouraging this type of physician support may be a productive pathway for increasing activation. This may be particularly important for those at lower levels of activation, who not only engage in fewer health promoting behaviors, but also tend to be passive with regard to their health care. These individuals are particularly at risk for declines in health and inadequate health care. That less-activated individuals are disproportionately represented in racial and ethnic minority groups suggests that attention to this attribute is a possible avenue to closing some of the racial and ethnic disparities in health.
Perhaps the main question for policy makers is what—if anything—can be done from a policy perspective to increase levels of patient activation. Because activation is changeable and provider support appears to be a factor, incentivizing or holding health care delivery systems and providers accountable for patient gains in activation is a possible policy direction.
In particular, some models of delivery are more amendable to supporting patient activation than others. For example, the medical home model, where patient-centered care is the focus and where a functioning medical team provides coordinated care, customizing care to support activation is possible. Similarly, in community health centers, where there are dedicated staff for supporting patient self-management, explicit support for activation could be provided.
On the other hand, the study results should give pause to policy makers who are promoting consumer-directed health care in the Medicaid program. For example, Indiana became the first state in 2008 to implement a high-deductible plan and health savings account program for some uninsured and Medicaid enrollees under the President’s Affordable Choices Initiative. Other states, including Florida, West Virginia, Kentucky and South Carolina, also have experimented with various types of consumer-directed care models in their Medicaid programs, with the objective of incentivizing enrollees to take more responsibility—and risks—for their health care utilization.
However, people enrolled in Medicaid are among the least-activated patients among all insurance groups, which reflects both lower educational levels and lower socioeconomic status. The findings suggest that efforts to increase patient responsibility in the Medicaid program will only succeed if they are accompanied by vigorous efforts to educate enrollees and increase their levels of activation.
The data for this report are from the HSC 2007 Health Tracking Household Survey, a nationally representative telephone survey of the civilian noninstitutionalized U.S. population sponsored by the Robert Wood Johnson Foundation. The sample includes about 17,800 persons, including about 15,500 adults age 18 and over. The response rate for the survey was 43 percent. Population weights adjust for probability of selection and differences in nonresponse based on age, sex, race/ethnicity and education. Information was obtained on all adults in the family as well as a randomly selected child.
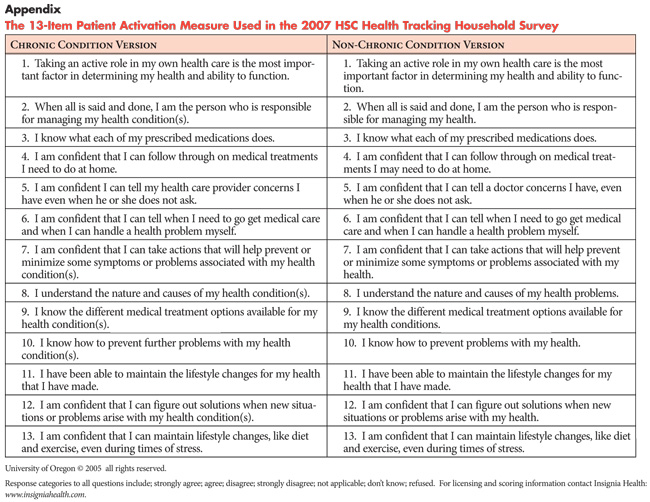
The 13-item Patient Activation Measure (PAM) was asked of all adults age 18 and over and was self-reported. Although the PAM was originally designed to be used for persons with chronic conditions, a slightly modified version was developed for persons with no chronic conditions (see Appendix). Persons in the survey were asked whether they had one or more of 10 common chronic conditions, including diabetes, arthritis, asthma, chronic obstructive pulmonary disease, hypertension, other heart disease, cancer, skin cancer, depression or uterine bleeding. Persons who reported one or more of these conditions were asked the original PAM version (i.e. for persons with chronic conditions), while those who did not have any of the 10 conditions were asked the modified PAM questions (i.e. for persons with no chronic conditions).
Both versions of the PAM questions use Likert-type response categories, including strongly agree, agree, disagree and strongly disagree. Persons who reported “not applicable,” “don’t know” or “refused” on more than half of the PAM scale items (7 or more) were dropped from the analysis. In addition, persons who replied “strongly agree” or “strongly disagree” on all 13 items were considered outliers and also excluded from the analysis. After these omissions, responses for about 13,500 adults were used to construct the PAM scale. Construction of the scale involved computing a “raw score” by summing the responses to all 13 questions. For persons who were missing one or more PAM items, the raw score was obtained by dividing the sum of the scores for the non-missing items by the number of non-missing items. Using the established methodology for the PAM, an activation score from 0-100 was assigned to each person based on their raw score.
Identifying levels of activation is based on whether an activation score falls within a previously determined range of scores. Level 1, the lowest level of activation, includes activation scores of 47 or lower; Level 2 includes scores of 47.1 to 55.1; Level 3 includes scores of 55.2 to 67.0; and Level 4 (the highest activation level) includes scores of 67.1 or above.
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org