
Issue Brief No. 131
April 2010
Ann S. O'Malley, Genna R. Cohen, Joy M. Grossman
Commercial electronic medical records (EMRs) both help and hinder physician interpersonal communication—real-time, face-to-face or phone conversations—with patients and other clinicians, according to a new Center for Studying Health System Change (HSC) study based on in-depth interviews with clinicians in 26 physician practices. EMRs assist real-time communication with patients during office visits, primarily through immediate access to patient information, allowing clinicians to talk with patients rather than search for information from paper records. For some clinicians, however, aspects of EMRs pose a distraction during visits. Moreover, some indicated that clinicians may rely on EMRs for information gathering and transfer at the expense of real-time communication with patients and other clinicians. Given time pressures already present in many physician practices, EMR and office-workflow modifications could help ensure that EMRs advance care without compromising interpersonal communication. In particular, policies promoting EMR adoption should consider incorporating communication-skills training for medical trainees and clinicians using EMRs.
![]() ffective interpersonal communication—real-time, face-to-face
or phone conversations—allows clinicians—physicians, nurses and other
practitioners—to acquire nuanced information from patients and other clinicians
that cannot easily be communicated in medical records, including social context,
values, preferences and issues specific to complex patients.1
Better communication between patients and physicians and between primary care
physicians and specialists is a key component of care coordination and leads
to improved patient outcomes.2-4 Yet, patients’ and clinicians’
levels of satisfaction with interpersonal communication have declined.5,
6
ffective interpersonal communication—real-time, face-to-face
or phone conversations—allows clinicians—physicians, nurses and other
practitioners—to acquire nuanced information from patients and other clinicians
that cannot easily be communicated in medical records, including social context,
values, preferences and issues specific to complex patients.1
Better communication between patients and physicians and between primary care
physicians and specialists is a key component of care coordination and leads
to improved patient outcomes.2-4 Yet, patients’ and clinicians’
levels of satisfaction with interpersonal communication have declined.5,
6
Interpersonal communication includes both patient-clinician communication, which is part of an ongoing relationship, and communication between clinicians, which primarily involves discussing clinical decisions for shared patients.7 EMRs can potentially support both types of communication.
While EMRs are expected to improve information sharing, it is less clear how their actual use affects interpersonal communication. This topic is particularly timely given the recent federal push for widespread EMR adoption,8 and the need to avoid worsening already-poor communication with patients and between clinicians sharing responsibility for patients. To this end, 52 physicians and other staff at 26 small and medium-sized physician practices with commercial ambulatory EMRs in place for at least two years were interviewed in-depth about the impact of EMRs on communication with patients and other clinicians as part of a study about the overall impact of EMRs on coordination of care.9 Additional interviews were conducted with chief medical officers at four EMR vendors and four national experts active in health information technology implementation (see Data Source).
![]() linicians believed EMRs facilitated communication with
patients in a variety of ways (see Table 1). In general,
immediate access to EMR data enabled them to focus on the patient rather than
gathering information from a variety of paper sources during visits. As one
physician explained, because “we do not have to call down the hall for a lab
or test result, we spend more quality time [with the patient] in a more context-rich
way.” Similarly, because staff can pose questions to the physicians via the
EMR’s electronic instant messaging (IM) function, rather than opening the exam
room door, doctor-patient communication during a visit can continue uninterrupted,
at least physically.
linicians believed EMRs facilitated communication with
patients in a variety of ways (see Table 1). In general,
immediate access to EMR data enabled them to focus on the patient rather than
gathering information from a variety of paper sources during visits. As one
physician explained, because “we do not have to call down the hall for a lab
or test result, we spend more quality time [with the patient] in a more context-rich
way.” Similarly, because staff can pose questions to the physicians via the
EMR’s electronic instant messaging (IM) function, rather than opening the exam
room door, doctor-patient communication during a visit can continue uninterrupted,
at least physically.
Ease of access to information also enriched patient education during visits. For example, clinicians could pull up information from the patient’s record, such as the problem list, medication list and care plan, or educational information from the Internet to review on screen with patients and family members during the visit. Some respondents reported sharing copies of that information with the patient/family to reinforce their discussion.
While not real-time communication, e-mail had a perceived impact on the timeliness of interpersonal communication. Clinicians who used EMRs’ e-mail function with patients generally believed e-mail “lowered communication barriers” and “improved the quality of the relationship” by enhancing access between visits and reducing phone tag. Illustrating how e-mail increased the likelihood of opening doors to communication at key times, one internist reported, “My favorite example is getting a letter from a doctor telling me that the patient I sent to him has a new diagnosis. we want to reach out to the patient at that moment, but we’ll probably have a pretty high threshold for making a phone call because it starts a telephone game. Now, I will routinely send the patient an e-mail saying, ‘I got this information [from the specialist who gave you this diagnosis]; I’m here for you if you want to talk.’ I think patients love that.”
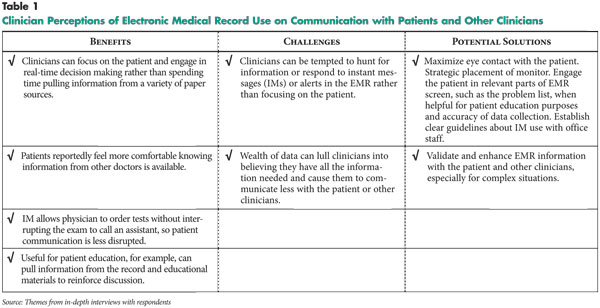
![]() espondents also noted EMRs could pose challenges to interpersonal communication. For example, using a computer during a patient visit can be a distraction—as one physician put it, “It’s like having a two-year old in the room.” As another physician observed, “. there are a lot of gadgets and gizmos and that can pull us away from our objective.” Instant messages, though valuable for communicating efficiently about care tasks and minimizing physical interruptions of visits, can distract clinicians from the patient if clinicians cannot adequately manage or ignore IM alerts in the exam room.
espondents also noted EMRs could pose challenges to interpersonal communication. For example, using a computer during a patient visit can be a distraction—as one physician put it, “It’s like having a two-year old in the room.” As another physician observed, “. there are a lot of gadgets and gizmos and that can pull us away from our objective.” Instant messages, though valuable for communicating efficiently about care tasks and minimizing physical interruptions of visits, can distract clinicians from the patient if clinicians cannot adequately manage or ignore IM alerts in the exam room.
Ironically, EMRs have enabled some clinicians to engage less with patients because, relative to paper charts, so much more information is available before actually seeing the patient. As one internist said, “. my concern now is that we’re listening less because we have more information when we walk in the room, and it’s not all trustworthy.” Another internist, who works in both outpatient and inpatient settings, noted his fear that EMRs could greatly diminish real-time communication with patients, “A lot of us feel like we’re already seeing it. . One of the hospitalists yesterday said ‘This is great, I used the EMR before I came here. I was able to sit down with my bagel and coffee and do my rounds before I even got in.’”
Some physicians also observed that because of EMR design elements, the temptation to focus on filling out checkboxes in the EMR reduced the amount of open-ended questions they ask patients. There are benefits from encouraging clinicians to more routinely ask about particular elements of patients’ histories and ideally entering structured and coded data that is searchable. However, exclusive use of checkboxes in taking a patient history risks that subtle or nuanced symptoms might go unidentified.
Experienced EMR users cited several ways to prevent EMRs from diminishing interpersonal communication with patients. For example, several physicians remarked that showing patients portions of their records could facilitate more accurate documentation and joint decision making, while helping to avoid a sense of alienation for patients while the physician looks at the computer screen. Noting that it helps ensure complete and accurate documentation, one physicians said, “Before I examine a patient, [we] sit down and look at the problem list and the medication list together. it provides a nice triangular interaction” between the physician, the computer and the patient.
![]() lectronic medical records provide quick access to patient information, enabling real-time communication about patients when a physician responds to phone inquiries from other clinicians. As one primary care physician said, “I know I can now so easily and quickly give information to specialists who call.”
lectronic medical records provide quick access to patient information, enabling real-time communication about patients when a physician responds to phone inquiries from other clinicians. As one primary care physician said, “I know I can now so easily and quickly give information to specialists who call.”
EMRs also foster a feeling among clinicians that patient information is a shared asset when they co-manage patients, as opposed to something one practice “owns.” A national expert commented that this improves interpersonal communication between clinicians because “EMRs move physicians away from the concept that, it [patient information] is mine and you can’t look at it. It should be shared for teaching and management purposes in a secure way.”
![]() ust as EMRs can tempt a clinician to disengage from patients, they also can detract from communication within a practice or between clinicians. The use of asynchronous EMR communication tools, such as e-mail and instant messaging where there is a time lag between responses, can be a double-edged sword, according to respondents.
ust as EMRs can tempt a clinician to disengage from patients, they also can detract from communication within a practice or between clinicians. The use of asynchronous EMR communication tools, such as e-mail and instant messaging where there is a time lag between responses, can be a double-edged sword, according to respondents.
On the one hand, most respondents believed that tools such as IM, “tasking”—assigning responsibility for a particular task to a staff member via the EMR—and e-mail increased efficiency for communications that do not require face-to-face interactions with staff, such as scheduling a follow-up visit. On the other hand, some respondents reported that the convenience of asynchronous communication in EMRs decreased the likelihood that real-time communication would occur when needed most, for example, during patient emergencies. One physician explained the importance of discussing with staff the types of urgent or sensitive issues that should be communicated orally, such as notifying a physician about a patient’s arrival at the emergency department. “You have to use electronic communication when appropriate and voice when appropriate, and even paper when it’s appropriate,” he said.
Another example was cited by one physician, “People will [use electronic communication] instead of knocking on the door or walking across the hall. You might not see your partner all day, whereas in the old days, we would ask what they think.”
For complicated patient situations, respondents believed nothing should replace the interactive aspects of face-to-face or phone conversations. As a cardiologist said, “If I am implanting a defibrillator, the primary care physician may have some thoughts about the patient’s true life expectancy that might influence our decision-making process about whether the device is appropriate for the patient. we need to do a better job [of communicating orally], because we [cardiologists] can’t do it without input from the physicians that understand the patient’s complex chronic conditions.”
EMR users cited several approaches to prevent EMRs from diminishing interpersonal communication with other clinicians and staff. For example, setting clear expectations with office staff on what is appropriate for electronic vs. oral communication is important. As several respondents noted, clinicians need to remind themselves, and the students and medical residents they help train, about the importance of face-to-face or phone conversations when indicated. As an EMR vendor and practicing physician noted, “The best way to ensure good coordination of care is for two physicians to speak with each other directly. You can’t approach any technology solution, in as complex and risky a work environment as the practice of medicine, and have it be a substitute for appropriate human interactions.”
![]() thers have found that EMR and computerized physician order
entry users have overly optimistic expectations regarding data accuracy and
processing.10 EMRs, like paper records, may contain inaccuracies;
reports of providers’ categorical reliance on this information highlight the
need to encourage users to verify EMR information directly with patients as
they would with a paper chart.
thers have found that EMR and computerized physician order
entry users have overly optimistic expectations regarding data accuracy and
processing.10 EMRs, like paper records, may contain inaccuracies;
reports of providers’ categorical reliance on this information highlight the
need to encourage users to verify EMR information directly with patients as
they would with a paper chart.
Use of an EMR has been noted in some studies to result in less face-to-face engagement with patients, making it more difficult for clinicians to focus their attention on particular aspects of patient-centered communication, such as outlining the patient’s agenda, exploring psychosocial and emotional issues, discussing how health problems affect a patient’s life, and ascertaining the timing of events needed to assess patients’ problems.11-13
On the other hand, a national survey of physicians14 and a study of patients15 found that EMRs in the exam room had either a neutral or positive impact on perceptions of patient-physician communication in terms of overall quality of communication about medical issues and psychosocial issues. Others have found that how computers are used in the exam room may depend on a clinician’s baseline patient-communication skills before EMR adoption.16 Different findings from these studies likely reflect their measurement of different aspects of communication, but the variation points to the need to develop a better understanding of how specific aspects of interpersonal communication are influenced by EMR use.
![]() ccording to physicians currently using commercial EMRs, the technology can both help and hinder communication with patients and other clinicians. These findings have implications for the support and training of professionals about interpersonal-communication skills in the presence of EMRs.
ccording to physicians currently using commercial EMRs, the technology can both help and hinder communication with patients and other clinicians. These findings have implications for the support and training of professionals about interpersonal-communication skills in the presence of EMRs.
Insufficient communication between physicians about shared patients results in part from the lack of payment for these kind of coordination activities and related opportunity costs associated with phone or face-to-face conversations that can disrupt the flow of office visits.17 EMRs and associated electronic communication tools can help address this problem by facilitating information sharing. However, real-time communication will continue to be important in many cases, and increased use of EMRs and electronic communication, if not properly managed, may undermine interpersonal communication. To this end, policy makers might consider incentives for communication among clinicians about shared patients.
Overcoming EMR-related challenges to interpersonal communication will likely involve continued refinement of their design by vendors and use by clinicians to decrease the potential for distraction during the patient encounter. Efforts around health information technology implementation at the federal and clinical practice level might incorporate training to improve interpersonal communication skills for practitioners and medical trainees in the presence of an EMR. The modification of office processes and clinical workflows to maximize interpersonal communication while using an EMR is also likely to be helpful.
A total of 60 telephone interviews were conducted from January-August 2008 with 52 clinicians in primary care and specialty practices with commercial ambulatory care EMRs in place for at least two years, four national experts, and four EMR vendor medical directors. Practices, ranging in size from solo to large groups, were identified within the 12 randomly selected Community Tracking Study (CTS) markets across the United States. Respondents were asked how they felt about EMRs’ impact on their interpersonal communication with: 1) patients; 2) clinicians and staff within their office; and 3) physicians in other practices. We were not able to validate respondents’ perceptions with direct measures of actual communication, for example, by audio-taping encounters. Additional details on the methodology, including participant recruitment, data collection and analysis have been previously published.18
This study was funded by The Commonwealth Fund.
Thanks as well to the state and local physicians societies, in particular the Massachusetts Medical Society, and the state and local chapters of the American College of Physicians (ACP), the American Academy of Family Physicians (AAFP), the American Society of Clinical Oncologists (ASCO), and the American College of Cardiology (ACC), that helped us identify and contact practices in the 12 CTS markets. We are especially grateful to the numerous anonymous physicians, practice staff and experts who generously gave their time to be interviewed for this project. Their input was invaluable.
RESEARCH BRIEFS are published by the Center for Studying Health System
Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org