
Issue Brief No. 134
October 2010
Ellyn R. Boukus, Joy M. Grossman, Ann S. O'Malley
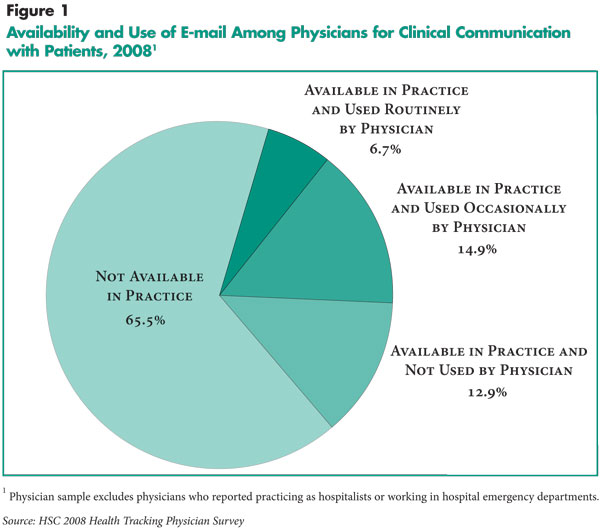
Some experts view e-mail between physicians and patients as a potential tool to improve physician-patient communication and, ultimately, patient care. Despite indications that many patients want to e-mail their physicians, physician adoption and use of e-mail with patients remains uncommon—only 6.7 percent of office-based physicians routinely e-mailed patients in 2008, according to a new national study from the Center for Studying Health System Change (HSC). Overall, about one-third of office-based physicians reported that information technology (IT) was available in their practice for e-mailing patients about clinical issues. Of those, fewer than one in five reported using e-mail with patients routinely; the remaining physicians were roughly evenly split between occasional users and non-users. Physicians in practices with access to electronic medical records and those working in health maintenance organizations (HMOs) or medical school settings were more likely to adopt and use e-mail to communicate with patients compared with other physicians. However, even among the highest users—physicians in group/staff-model HMOs—only 50.6 percent reported routinely e-mailing patients.
![]() -mail between physicians and patients is viewed by some as a way to enhance communication, increase patient engagement and satisfaction, improve patient outcomes and quality of care, and boost efficiency. Some recent studies have demonstrated positive impacts of patient-provider e-mail across all of these dimensions, although the research is typically focused on narrow subsets of patients, such as diabetics, or limited to a specific practice setting, such as an integrated delivery system.1 Moreover, public opinion polls suggest that patients are ready and willing to communicate with their physicians via e-mail. One survey, conducted at the end of 2009, found that between 50 percent and 70 percent of adults who did not use e-mail to communicate with their doctors or nurses were interested in doing so.2 Nonetheless, only 8 percent of all of the adults surveyed reported ever sending an e-mail to or receiving an e-mail from their doctor.3
-mail between physicians and patients is viewed by some as a way to enhance communication, increase patient engagement and satisfaction, improve patient outcomes and quality of care, and boost efficiency. Some recent studies have demonstrated positive impacts of patient-provider e-mail across all of these dimensions, although the research is typically focused on narrow subsets of patients, such as diabetics, or limited to a specific practice setting, such as an integrated delivery system.1 Moreover, public opinion polls suggest that patients are ready and willing to communicate with their physicians via e-mail. One survey, conducted at the end of 2009, found that between 50 percent and 70 percent of adults who did not use e-mail to communicate with their doctors or nurses were interested in doing so.2 Nonetheless, only 8 percent of all of the adults surveyed reported ever sending an e-mail to or receiving an e-mail from their doctor.3
While patients appear ready to embrace e-mail, physicians are markedly less ready, according to findings from the nationally representative HSC 2008 Health Tracking Physician Survey. Only 34.5 percent of U.S. physicians providing office-based ambulatory care in 2008 reported that information technology for communicating with patients about clinical issues via e-mail was available in their practice (see Figure 1 and Data Source). Of the physicians with access to e-mail, fewer than one in five (19.5%) routinely used e-mail to communicate about clinical issues with patients. Overall, only 6.7 percent of all office-based physicians nationally routinely e-mailed patients in 2008. In contrast, use of e-mail to communicate with other providers was more common: twice as many physicians spent at least some time each work day e-mailing physicians and other clinicians compared with e-mailing patients and their families (findings not shown).
![]() hysician concerns about lack of reimbursement, the potential for increased workload, maintaining data privacy and security, avoiding increased medical liability, and the uncertain impact on care quality are commonly cited as reasons why physicians may be reluctant to use e-mail.4 Policy makers are actively considering ways to promote the use of secure online communications between physicians and patients, for example, through support of the patient-centered medical home model or through Medicare and Medicaid payment incentives for “meaningful use” of health IT.
hysician concerns about lack of reimbursement, the potential for increased workload, maintaining data privacy and security, avoiding increased medical liability, and the uncertain impact on care quality are commonly cited as reasons why physicians may be reluctant to use e-mail.4 Policy makers are actively considering ways to promote the use of secure online communications between physicians and patients, for example, through support of the patient-centered medical home model or through Medicare and Medicaid payment incentives for “meaningful use” of health IT.
The HSC survey asked about the availability in the physician’s practice of e-mail to communicate with patients but did not ascertain what specific types of e-mail tools were available. Policy makers are focused on the adoption of secure electronic messaging that is compliant with the Health Insurance Portability and Accountability Act (HIPAA) privacy and security rules. The survey estimates, however, do not differentiate among a host of electronic communication tools that include both traditional unencrypted e-mail as well as secure Web-based messaging tools. The latter may be embedded in more sophisticated platforms, such as patient portals that support other functions, including prescription refill requests, online appointment scheduling or accessing medical records, and may or may not be linked with electronic medical record (EMR) systems.5 Some more technically sophisticated platforms also may support real-time, virtual consultations that can substitute for a face-to-face visit and go beyond patients and physicians sending and receiving messages without being online at the same time.6
The survey questions also did not ask whether other practice staff, aside from the physician, e-mailed with patients about clinical issues. Practices vary substantially in how electronic communication tools are implemented: in some practices, office staff may triage e-mail questions, limiting the number of messages to which the physician must directly respond.7 Consequently, the study results may underestimate the extent to which physician practice staff, more broadly, used electronic communication tools with patients.
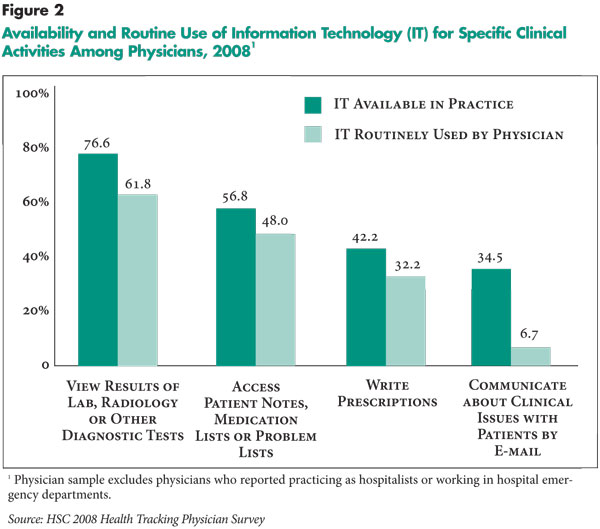
![]() he low prevalence of physician-patient e-mail becomes even more apparent when compared to other forms of IT in physician practices, especially given the low rates of health IT adoption among providers generally. Among 16 clinical tasks that can be supported by IT that physicians were asked about in the survey, e-mail communication with patients ranked third to last with respect to availability and last in terms of routine use (see Figure 2 for select clinical tasks). Almost 35 percent of all physicians had access to e-mail in their practice, while only 6.7 percent routinely used the technology. In contrast, 76.6 percent of physicians had IT for viewing results of laboratory and other diagnostic tests, and 61.8 percent routinely used the technology.
he low prevalence of physician-patient e-mail becomes even more apparent when compared to other forms of IT in physician practices, especially given the low rates of health IT adoption among providers generally. Among 16 clinical tasks that can be supported by IT that physicians were asked about in the survey, e-mail communication with patients ranked third to last with respect to availability and last in terms of routine use (see Figure 2 for select clinical tasks). Almost 35 percent of all physicians had access to e-mail in their practice, while only 6.7 percent routinely used the technology. In contrast, 76.6 percent of physicians had IT for viewing results of laboratory and other diagnostic tests, and 61.8 percent routinely used the technology.
Physicians in practices equipped with fully electronic EMRs were more than twice as likely to report having access to e-mail and were more than three times as likely to use it routinely to communicate with patients when available, compared with physicians in practices using paper records exclusively (see Table 1). While physician-patient e-mail tools have not typically been part of the core functionality of EMR systems, practices with EMRs can implement add-on secure messaging tools or multi-function patient portals. Integrating patient communication tools with EMRs can be challenging, but having an EMR may support more efficient and effective e-mail use and documentation in the patient’s medical record than using e-mail tools on a stand-alone basis with paper charts.8 The added convenience may help to prevent e-mail from becoming simply another inbox for physicians to check for incoming messages. EMR use in the practice may also signal greater physician comfort with and willingness to use other clinical IT, including e-mail, with patients.
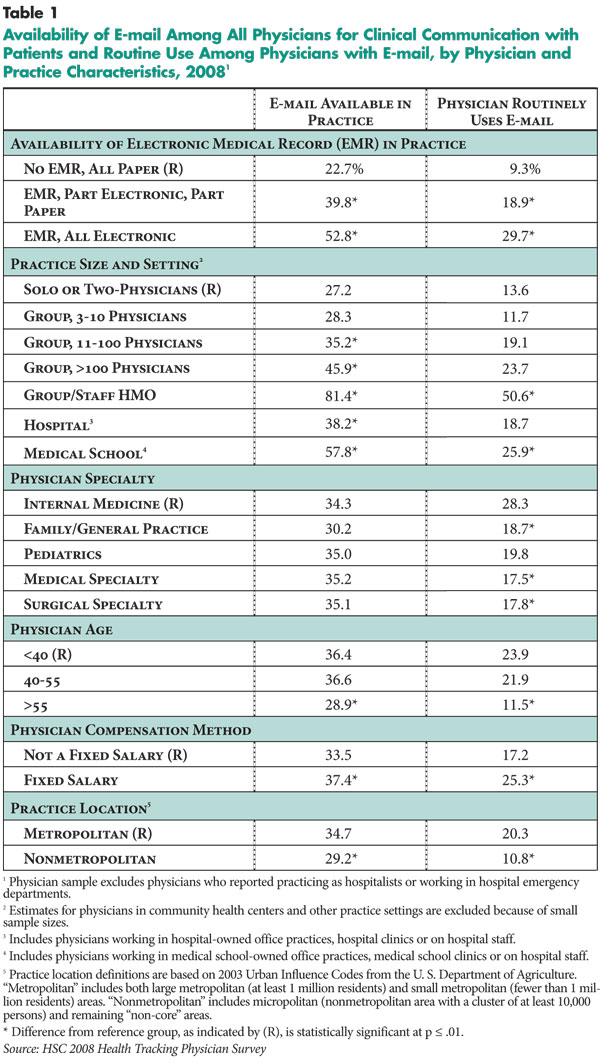
![]() hile availability of e-mail increases with practice size, there was little variation in routine use, except among physicians in group/staff model HMOs. This is in contrast to other types of health IT, such as electronic prescribing, where both adoption and use vary by practice settings.9 Even in HMOs, where more than 81 percent of physicians reported that e-mail was available in their practices, only about half of those physicians used it routinely. In contrast, in solo and two-physician practices, 27.2 percent of physicians reported e-mail was available, and of those, only 13.6 percent used it routinely. Medical school-based physicians also were more likely to have e-mail access (57.8%) and use it routinely when available (25.9%) compared with physicians in solo and two-physician practices, but the differences were less pronounced than for physicians working in HMOs.
hile availability of e-mail increases with practice size, there was little variation in routine use, except among physicians in group/staff model HMOs. This is in contrast to other types of health IT, such as electronic prescribing, where both adoption and use vary by practice settings.9 Even in HMOs, where more than 81 percent of physicians reported that e-mail was available in their practices, only about half of those physicians used it routinely. In contrast, in solo and two-physician practices, 27.2 percent of physicians reported e-mail was available, and of those, only 13.6 percent used it routinely. Medical school-based physicians also were more likely to have e-mail access (57.8%) and use it routinely when available (25.9%) compared with physicians in solo and two-physician practices, but the differences were less pronounced than for physicians working in HMOs.
The greater prevalence and—in some cases—use of e-mail among physicians in large group, group/staff HMOs and medical school practices may be related, in part, to other factors such as the higher rate of EMR adoption in those settings. However, differences in e-mail adoption and use remained even after considering only physicians in practices that use EMRs exclusively (findings not shown).
Generally, larger practices, particularly when part of integrated delivery systems, are more likely to have the resources to invest in technological innovations designed to improve workflow and transform ambulatory care delivery. For instance, large group/staff-model HMOs, such as Kaiser Permanente and Group Health Cooperative, have implemented electronic messaging through patient portals.10
While there was little variation in adoption across specialties, general internists were more likely to use e-mail routinely compared with other specialists. Compared with their younger counterparts, physicians older than 55 were less likely to have e-mail available, and those who had it were about half as likely to use it routinely for communicating with patients. This may reflect both age and work environment, since older physicians commonly work in smaller practices, which are less likely to be equipped with IT. Considering smaller and larger practices separately, when comparing physicians across age groups there were no differences in adoption, yet, on average, older physicians remained approximately half as likely to use e-mail routinely as younger physicians (findings not shown). This may reflect the fact that decisions about technology adoption are made at the practice level, while the choice of whether or not to use it may be left to individual physicians.
Financial incentives also may play a role in encouraging or discouraging the use of e-mail: physicians who received a fixed salary used e-mail more frequently than physicians who were compensated by other means. Physicians who are paid a fixed salary may communicate more with patients generally, including via e-mail, because they can devote more time to activities that are not directly reimbursed, compared with physicians who face practice revenue or productivity incentives. While physicians in larger practices and group/staff-model HMOs were more likely to receive a fixed salary, these differences in e-mail use remained after taking practice size and setting into account.
Patients in nonmetropolitan areas who have to commute long distances to obtain care may benefit particularly from e-mail interactions because of their potential to save travel time. However, physicians working in nonmetropolitan areas were less likely to have access to e-mail and about half as likely to use it routinely when it was available compared with providers in metropolitan areas. This may, in part, reflect differences in practice size, setting and available resources. Yet, these differences persisted even after accounting for the fact that physicians in nonmetropolitan areas were less likely to work in larger practices or have EMRs available.
![]() hysician concerns about increased workload without reimbursement, uncertainty about impacts on quality of care, and challenges related to data privacy and security and medical liability have hindered adoption and use of e-mail to communicate with patients. Federal policy efforts currently underway to support delivery system reforms may help spur physician adoption and use of e-mail communication with patients indirectly.
hysician concerns about increased workload without reimbursement, uncertainty about impacts on quality of care, and challenges related to data privacy and security and medical liability have hindered adoption and use of e-mail to communicate with patients. Federal policy efforts currently underway to support delivery system reforms may help spur physician adoption and use of e-mail communication with patients indirectly.
In July 2010, the Centers for Medicare and Medicaid Services and the Office of the National Coordinator for Health Information Technology released final rules to implement provisions of the America Recovery and Reinvestment Act of 2009 regarding Medicare and Medicaid incentive payments tied to the “meaningful use” of EMRs. While the incentives are not currently linked specifically to electronic communication with patients, growth in EMR use as a result of the incentives may at least indirectly encourage e-mail adoption and use to the extent electronic messaging tools are integrated or used in conjunction with EMRs, for the reasons described previously.
The Medicare and Medicaid incentive programs also require that physicians use EMRs that comply with standards to support privacy and safeguard personal health information. To the extent that electronic communication is tied with EMR use, these standards may help to allay physicians’ fears about data security. Finally, formal protocols governing message triaging, turnaround time, appropriate use and documentation can help to address physicians’ liability concerns.11
While EMRs may support the adoption of e-mail—and findings from the 2008 Health Tracking Physician Survey suggest that the two are indeed related—this is not a guaranteed outcome. Moreover, the question remains whether physicians will actually use e-mail in the absence of additional reimbursement for the extra costs required to communicate with patients via e-mail to better coordinate patient care.12 As Medicare and Medicaid “meaningful use” requirements increase as planned in later stages of the program’s implementation, policy makers may revisit earlier proposals to require the adoption of secure patient-provider messaging capabilities to receive future incentives.13 Expectation of these requirements may encourage some practices to adopt electronic communication sooner rather than later.
In the meantime, some health plans and physician practices have begun to explore different payment schemes to encourage e-mail communication with patients. Aetna and CIGNA are reimbursing providers nationwide for virtual visits, or “e-visits,” including the use of secure messaging and real-time online consults, on a per-visit basis.14 Another option is to reimburse providers on a capitated, or set fee per patient, basis for engaging in a broader set of care coordination activities that enhance communication with patients, as envisioned in the patient-centered medical home.15 Another approach is to charge patients annual fees for access to e-mail consults with physicians. Patients might be willing to underwrite the additional cost in return for time and travel savings and increased convenience. Moreover, the cost of electronic correspondence might be lower than what patients would pay for a face-to-face visit.16
Finally, policy makers and researchers might more systematically explore whether e-mail or other secure electronic communication with patients can deliver on its promise to enhance communication, increase patient engagement and satisfaction, improve patient outcomes and quality of care, and boost efficiency. If e-mail does achieve these goals, expanding incentives to encourage e-mail communication between physicians and patients might be a worthwhile investment
| 1. | 1. Houston, Thomas K., et al., “Experiences of Patients Who Were Early Adopters of Electronic Communication With Their Physician: Satisfaction, Benefits, and Concerns,” American Journal of Managed Care, Vol. 10, No. 9 (September 2004); Harris, Lynne T., et al., “Diabetes Quality of Care and Outpatient Utilization Associated with Electronic Patient-Provider Messaging: A Cross-Sectional Analysis,” Diabetes Care, Vol. 32, No. 7 (July 2009); Rosen, Paul, and C. Kent Kwoh, “Patient-Physician E-mail: An Opportunity to Transform Pediatric Health Care Delivery,” Pediatrics, Vol. 120, No. 4 (October 2007); Liederman, Eric M., et al., “The Impact of Patient-Physician Web Messaging on Provider Productivity,” Journal of Healthcare Information Management, Vol. 19, No. 2 (Spring 2005). |
| 2. | Fifty percent of adults who did not use personal health records (PHRs) were somewhat or very interested in sending an e-mail to, or getting an e-mail from, a doctor or nurse. Sixty-nine percent of adult PHR users who hadn’t done so were interested in this feature. See California HealthCare Foundation, Consumers and Health Information Technology: A National Survey (April 2010). |
| 3. | Ibid. |
| 4. | Katz, Steven J., and Cheryl A. Moyer, “The Emerging Role of Online Communication Between Patients and Their Providers,” Journal of General Internal Medicine, Vol. 19, No. 9 (September 2004). |
| 5. | Dixon, Ronald F., “Enhancing Primary Care Through Online Communication,” Health Affairs, Vol. 29, No. 7 (July 2010). |
| 6. | Whitten, Pamela, Lorraine Buis and Brad Love, “Physician-Patient e-Visit Programs: Implementation and Appropriateness,” Disease Management and Health Outcomes, Vol. 15, No. 4 (2007). |
| 7. | McCarthy, Douglas, Kimberly Mueller and Ingrid Tillman, Group Health Cooperative: Reinventing Primary Care by Connecting Patients with a Medical Home, Commonwealth Fund (July 2009). |
| 8. | California HealthCare Foundation, Online Patient-Provider Communication Tools: An Overview (November 2003). |
| 9. | Grossman, Joy M., Even When Physicians Adopt E-Prescribing, Use of Advanced Features Lags, Issue Brief No. 133, Center for Studying Health System Change, Washington, D.C. (July 2010). |
| 10. | Harris, et al. (2009); Chen, Catherine, et al., “The Kaiser Permanente Electronic Health Record: Transforming and Streamlining Modalities of Care,” Health Affairs, Vol. 28, No. 2 (March/April 2009). |
| 11. | American Medical Association, Guidelines for Physician-Patient Electronic Communication, http://www.ama-assn.org (accessed on Sept. 3, 2010). |
| 12. | Katz and Moyer (2004). |
| 13. | U.S. Department of Health and Human Services, Health IT Policy Council Recommendations to National Coordinator for Defining Meaningful Use (August 2009). |
| 14. | Gearon, Christopher J., “Take Two and E-mail Me at Your Convenience,” AHIP Coverage (July/August 2008). |
| 15. | Patient-Centered Primary Care Collaborative, Joint Principles of the Patient Centered Medical Home (February 2007). |
| 16. | Lowes, Robert, “Getting Paid for Mouse Calls,” Physicians Practice (March 2009); Dixon (2010). |
This Issue Brief presents findings from the HSC 2008 Health Tracking Physician Survey, a nationally representative mail survey of U.S. physicians. The sample of physicians was drawn from the American Medical Association master file and included active, nonfederal, office- and hospital-based physicians providing at least 20 hours per week of direct patient care. Residents and fellows were excluded, as were radiologists, anesthesiologists and pathologists. The survey includes responses from more than 4,700 physicians and had a 62 percent response rate. Because this Issue Brief focuses on use of e-mail in the outpatient setting, physicians reporting that they practice as hospitalists or treat patients in hospital emergency departments were excluded from this study. The resulting sample is 4,258 physicians. Estimates from this survey should not be compared to estimates from HSC’s previous Community Tracking Study Physician Surveys because of changes in survey administration mode from telephone to mail, question wording, skip patterns and sample structure.
Physicians were asked, “Is information technology available in your practice to communicate about clinical issues with patient by e-mail?” If the response was “yes,” physicians were further asked “How often do you personally use the technology?” The response categories provided were “routinely,” “occasionally” or “not at all.” Physicians were also asked, “Does your main practice use electronic medical records?” The response categories were “yes, all electronic,” “yes, part electronic and part paper,” and “no, all paper.”
More detailed information on survey content and methodology can be found at www.hschange.org.
The 2008 HSC Health Tracking Physician Survey and this research were funded by the Robert Wood Johnson Foundation.
ISSUE BRIEFS are published by the Center for Studying Health System
Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org