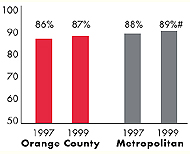
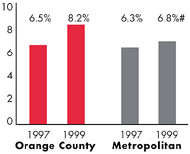
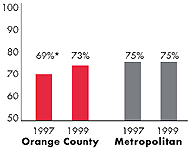
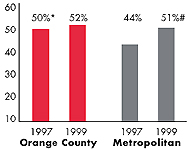
* Site value is significantly different from the mean for metropolitan
areas over 200,000 population.
# Statistically significant difference between 1997 and 1999 at p< .05.
The information in these graphs comes from the Household and Physician
Surveys conducted in 1996-1997 and 1998-1999 as part of HSC’s Community
Tracking Study.

