
Issue Brief No. 98
September 2005
Ha T. Tu, Peter J. Cunningham
In 2003, an estimated 13.5 million American children had special health care needs, ranging from learning disorders to severe disabilities. Medicaid or the State Children’s Health Insurance Program (SCHIP) covered nearly two out of five children with special health care needs, according to a new study by the Center for Studying Health System Change (HSC). Despite the critical safety net provided by public insurance to millions of special-needs children, an estimated 650,000 of these medically vulnerable children were uninsured in 2003. Many likely were eligible for public insurance but not enrolled. Among special-needs children, those with public and private coverage reported about equal rates of problems obtaining health care, indicating Medicaid and SCHIP provide access to care comparable to private insurance. Overall, children with special needs faced more access problems than other children, and their families reported more problems paying medical bills. Policy measures now under consideration, such as increased cost sharing in Medicaid and SCHIP, would likely increase access problems for children with special needs.
![]() bout 13.5 million children—or 18.5 percent of all
American children—had special health care needs in 2003, according to HSC’s
Community Tracking Study (CTS) Household Survey (see Data Source).
The term “children with special health care needs” was developed to identify
children with ongoing physical, emotional, behavioral, developmental or other
health conditions that cause them to use more health services or limit their
activities than children generally.1 The range of conditions
varies widely, ranging from learning disorders to severe disabilities.
bout 13.5 million children—or 18.5 percent of all
American children—had special health care needs in 2003, according to HSC’s
Community Tracking Study (CTS) Household Survey (see Data Source).
The term “children with special health care needs” was developed to identify
children with ongoing physical, emotional, behavioral, developmental or other
health conditions that cause them to use more health services or limit their
activities than children generally.1 The range of conditions
varies widely, ranging from learning disorders to severe disabilities.
Children with special health care needs are particularly reliant on adequate health insurance coverage. Public insurance programs—Medicaid and SCHIP—play a critical role in covering special-needs children. Nearly two in five special-needs children are enrolled in either Medicaid or SCHIP (see Figure 1).
Children with special needs are less likely than other children to have private insurance (55.6% vs. 63.6%). However, because they are enrolled in public insurance programs at much higher rates than other children, their uninsurance rate is lower—4.8 percent, compared with 8.3 percent for children without special needs.
However, an estimated 650,000 children with special health care needs were uninsured in 2003, and many were likely eligible for public health insurance but not enrolled.These findings counter the conventional wisdom that all uninsured children generally are healthy and that uninsured children eligible for public insurance would gain coverage if they became ill.
The special-needs children who are most likely to lack health insurance are those whose family incomes range from 100 percent to 300 percent of the federal poverty level—or $18,400 to $55,200 for a family of four in 2003. Special-needs children with family incomes between 100 percent and 200 percent of poverty have an uninsurance rate of 8.2 percent, while those with family incomes from 200 percent to 300 percent of poverty have an uninsurance rate of 9.8 percent (see Table 1).
In contrast, most of the special-needs children with family incomes below poverty have public coverage, leaving only 2.4 percent uninsured, while most of the those with family incomes exceeding 300 percent of poverty have private insurance, resulting in an uninsurance rate of just 1.6 percent.
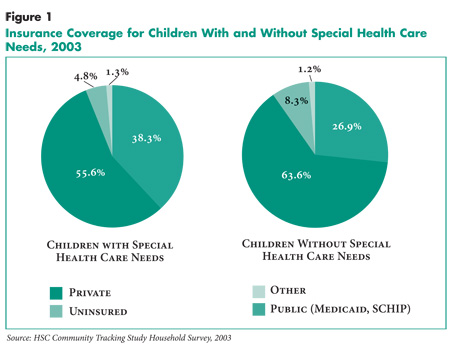 |
Table 1
|
|||
|
All Children
|
Children With Special Health Care Needs
|
Children Without Special Health Care Needs
|
|
| All Income Categories | |||
| Private Insurance |
62.1%
|
55.6%
|
63.6%*
|
| Public Insurance |
29.0
|
38.3
|
26.9*
|
| Uninsured |
7.7
|
4.8
|
8.3*
|
| Less than 100% of Poverty | |||
| Private Insurance |
14.0
|
9.7
|
15.2*
|
| Public Insurance |
71.4
|
86.9
|
67.2*
|
| Uninsured |
12.8
|
2.4
|
15.6*
|
| 100-199% of Poverty | |||
| Private Insurance |
43.1
|
32.7
|
45.2*
|
| Public Insurance |
45.2
|
57.6
|
42.6*
|
| Uninsured |
10.5
|
8.2
|
11.0*
|
| 200-299% of Poverty | |||
| Private Insurance |
75.0
|
59.5
|
78.6*
|
| Public Insurance |
15.9
|
28.0
|
13.1*
|
| Uninsured |
8.1
|
9.8
|
7.7
|
| 300% or More of Poverty | |||
| Private Insurance |
88.9
|
90.9
|
88.4*
|
| Public Insurance |
6.7
|
6.9
|
6.6
|
| Uninsured |
3.5
|
1.6
|
3.9*
|
| * Difference from children with special
health care needs is statistically significant at p <.05. Note: Children with other insurance coverage are not reported as a separate category due to small sample size but are included in totals for all children. Source: Community Tracking Study Household Survey, 2003 |
|||
![]() hildren with special needs are more likely than other children
to have a usual source of medical care: Only about one in 20 special-needs children
lacks a usual source of care, compared with one in 10 children without special
needs (see Table 2). It makes sense that children with
special needs are more likely to have a regular place to go to for care, because
their more frequent use of medical services would give their parents both greater
incentives and more opportunities to seek a medical home for them.
hildren with special needs are more likely than other children
to have a usual source of medical care: Only about one in 20 special-needs children
lacks a usual source of care, compared with one in 10 children without special
needs (see Table 2). It makes sense that children with
special needs are more likely to have a regular place to go to for care, because
their more frequent use of medical services would give their parents both greater
incentives and more opportunities to seek a medical home for them.
Even though special-needs children are more likely to have a usual source of care, they are almost twice as likely as other children to have had an unmet need for medical care in the past year (4.2% vs. 2.3%). And they are more than three times as likely to have had an unmet need for prescription drugs because of cost concerns in the past year (6.9% vs. 2.1%).
The access gaps faced by special-needs children relative to other children persist even among insured children. The pattern of special-needs children having more problems getting care holds for both privately and publicly insured children.
Comparing access for special-needs children across different insurance categories, special-needs children covered by Medicaid or SCHIP appear to have no more problems getting care than those with private coverage. This indicates that public coverage provides access to care for special-needs children comparable to what special-needs children with private coverage receive.
Access to care for uninsured children with special needs cannot be reported separately because the survey did not contain information on enough uninsured special-needs children to yield reliable estimates. However, a comparison of all uninsured children to all insured children reveals large access disparities and suggests that uninsured special-needs children face large access gaps relative to their insured counterparts.2
Table 2
|
|||
|
All Children
|
Children With Special Health Care Needs
|
Children Without Special Health Care Needs
|
|
| No Usual Source of Care |
8.6%
|
4.7%
|
9.5%#
|
| All Insurance |
6.6
|
3.4
|
7.4#
|
| Private Insurance |
5.0
|
2.5
|
5.5#
|
| Public Insurance |
9.7*
|
4.7
|
11.3*#
|
| Uninsured |
32.1*
|
NA
|
32.4*
|
| Unmet Need |
2.7
|
4.2
|
2.3#
|
| All Insurance |
2.3
|
4.0
|
1.9#
|
| Private Insurance |
2.0
|
4.0
|
1.6#
|
| Public Insurance |
2.9
|
3.6
|
2.7
|
| Uninsured |
7.2*
|
NA
|
7.0*
|
| Delayed Care |
3.7
|
5.3
|
3.4#
|
| All Insurance |
3.1
|
4.6
|
2.8#
|
| Private Insurance |
3.0
|
4.6
|
2.6
|
| Public Insurance |
3.2
|
4.7
|
2.7
|
| Uninsured |
11.6*
|
NA
|
10.6*
|
| Unmet Need for Prescription Drug Due to Cost |
3.0
|
6.9
|
2.1#
|
| All Insurance |
2.4
|
5.9
|
1.6#
|
| Private Insurance |
1.9
|
5.1
|
1.3#
|
| Public Insurance |
3.5
|
7.0
|
2.4
|
| Uninsured |
9.6*
|
NA
|
7.2*
|
| * Difference from privately insured is statistically
significant at p <.05. # Difference between children with and without special health care needs is statistically significant at p <.05. Notes: Estimates are not reported for uninsured special needs children due to small sample size. Children with other insurance coverage are not reported as a separate category due to small sample size, but are included in totals for all children and all insured children. Source: Community Tracking Study Household Survey, 2003 |
|||
![]() igher rates of access problems for children with special needs reflect greater need and use of health services, which can generate large out-of-pocket expenses and cause people to forgo or delay care because of cost concerns.
igher rates of access problems for children with special needs reflect greater need and use of health services, which can generate large out-of-pocket expenses and cause people to forgo or delay care because of cost concerns.
Special-needs children account for at least one-third of all ambulatory care visits and inpatient hospital stays made by children, although they comprise less than one-fifth of all children (see Supplementary Table 1). Given the heavier use of health services by special-needs children, it is not surprising that their families are more likely than other families to face higher out-of-pocket medical costs and to have more problems paying medical bills. Indeed, a quarter of all children with special needs are in families with medical bill problems, compared with 17 percent of children without special needs.
Families of special-needs children are more likely to have medical bill problems when they have low incomes, lack private insurance, have a special-needs child in fair or poor health, or include another family member with health problems (see Supplementary Tables 2a and 2b). It is noteworthy that families of special-needs children covered by Medicaid or SCHIP are almost twice as likely to have medical bill problems as families of privately insured special-needs children (32.2% vs. 17.3%)—a gap that largely reflects differences in family income but also reflects poorer health status among publicly insured special-needs children.
Children with special needs whose families have problems paying medical bills have a substantially harder time getting care (see Table 3). Although they are not significantly more likely to lack a usual source of care, they are much more likely to have forgone medical care (7.3% vs. 3.2%) and to have delayed medical care (9.8% vs. 3.8%), compared with special-needs children without family medical bill problems. The disparity in being able to obtain needed prescription drugs is most striking of all: Being in a family with medical bill problems made special-needs children more than three times as likely to have an unmet need for drugs because of cost (14.8% vs. 4.3%).
Table 3
|
|||
|
All Children With Special Health Care Needs
|
In Families With Medical Bill Problems
|
In Families Without Medical Bill Problems
|
|
| No Usual Source of Care |
4.7%
|
5.9%
|
4.3%
|
| Unmet Need |
4.2
|
7.3
|
3.2*
|
| Delayed Care |
5.3
|
9.8
|
3.8*
|
| Unmet Need for Prescription Drug Due to Cost |
6.9
|
14.8
|
4.3*
|
| * Difference from children in families with medical bill problems is statistically
significant at p <.05. Source: Community Tracking Study Household Survey, 2003 |
|||
![]() ith nearly two out of every five children with special health care needs relying on Medicaid or SCHIP, public insurance programs play a crucial role in ensuring access to health care services for these vulnerable children. Although access problems for special-needs children are higher than for other children, they would likely be even higher without insurance coverage.
ith nearly two out of every five children with special health care needs relying on Medicaid or SCHIP, public insurance programs play a crucial role in ensuring access to health care services for these vulnerable children. Although access problems for special-needs children are higher than for other children, they would likely be even higher without insurance coverage.
Most children covered by Medicaid and SCHIP are eligible for these programs solely because of low family incomes and have no more health problems than the average child. However, because Medicaid covers many high-need children through its disability and Medically Needy programs, publicly insured children include some of the most intensive users of health services among all children. Relative to privately insured special-needs children, for example, publicly insured special-needs children average more ambulatory visits and hospital stays. And among all children with public insurance, special-needs children consume a large share of health care resources: Even though special-needs children comprise less than a quarter of all publicly insured children, they account for almost half of all hospital stays made by publicly insured children.
Budget pressures have caused both the federal government and the states to explore ways to slow spending growth in public insurance programs. Although recent federal proposals to reduce Medicaid spending growth have focused mostly on eligibility and services for adults, during the past year some states have made it more difficult for eligible children to obtain and keep public coverage. These measures include increasing required premiums or targeting premiums to lower-income families in SCHIP, imposing enrollment freezes in SCHIP, and reinstating administrative barriers in both Medicaid and SCHIP.3
Even modest introductions of cost-sharing requirements where there typically have been none (as in Medicaid), or modest increases in cost sharing where they already exist (as in many SCHIP programs), can cause serious hardships for low-income families. Already, one-third of all publicly insured special-needs children are in families that have problems paying medical bills. That proportion is almost certain to increase if families of special-needs children covered by Medicaid and SCHIP are required to shoulder a larger share of health expenses.
Continuing or worsening budget pressures may lead policy makers to consider more cuts that affect special-needs children. Because the special-needs population includes intensive users of medical care who accumulate relatively high costs, efforts to trim costs from public programs may have to encompass these children. At the same time, these children are heavy users precisely because they are among the most medically needy, so even incremental cost-cutting measures may have significant negative impact on access to care. Policy makers seeking ways to control public spending will need to balance that priority with the need to provide adequate health care access and financial protection for the families of children with special health care needs.
This Issue Brief presents findings from the 2003 Community Tracking Study Household Survey, a nationally representative survey containing information on 46,600 persons. This analysis focuses on a sample of 7,327 children under 18 years of age, of whom 1,523 were identified as children with special health care needs.
The survey used the Children with Special Health Care Needs (CSHCN) Screener, a standardized five-question survey module developed by federal and state policy makers, health care providers, researchers and consumer organizations. The CSHCN Screener is non-condition specific and health consequence-based and is designed to reflect the Maternal and Child Health Bureau’s definition of children with special health care needs: “Children who have a. chronic physical, developmental, behavioral or emotional condition and who also require health and related services of a type or amount beyond that required by children generally.” For additional information, see the Foundation for Accountability, The Children with Special Health Care Needs (CSHCN) Screener at http://dch. ohsuhealth.com//index.cfm?cfid=6&cft oken=59572841&pageid=458§ionI D=133.
The CSHCN Screener is administered to parents and consists of five questions, each representing a specific health consequence: use or need of prescription medication; above average use or need of medical, mental health or educational services; functional limitations compared with others of same age; use or need of specialized therapies; and treatment or counseling for emotional or developmental problems. A child qualifies as having a special health care need if the parent responds “yes” to one of these five questions, and also responds “yes” to two follow-up questions: The consequence is due to a medical or other health condition; and the duration or expected duration of the condition is 12 months or longer.
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org