Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Insurers Consolidate, Hospitals Struggle Financially
Syracuse, New York
Community Report No. 05
Winter 2001
Aaron Katz, Robert E. Hurley, Leslie A. Jackson, Timothy K. Lake, Ashley C. Short, James D. Reschovsky
 n October 2000, a team of researchers
visited Syracuse, N.Y., to study that
community’s health system, how it is
changing and the effects of those
changes on consumers. The Center for
Studying Health System Change
(HSC), as part of the Community
Tracking Study, interviewed more than
60 leaders in the health care market.
Syracuse is one of 12 communities
tracked by HSC every two years
through site visits and surveys.
Individual community reports are
published for each round of site visits.
The first two site visits to Syracuse, in
1996 and 1998, provided baseline and
initial trend information against
which changes are tracked. The
Syracuse market includes Cayuga,
Madison, Onondaga and Oswego
counties. n October 2000, a team of researchers
visited Syracuse, N.Y., to study that
community’s health system, how it is
changing and the effects of those
changes on consumers. The Center for
Studying Health System Change
(HSC), as part of the Community
Tracking Study, interviewed more than
60 leaders in the health care market.
Syracuse is one of 12 communities
tracked by HSC every two years
through site visits and surveys.
Individual community reports are
published for each round of site visits.
The first two site visits to Syracuse, in
1996 and 1998, provided baseline and
initial trend information against
which changes are tracked. The
Syracuse market includes Cayuga,
Madison, Onondaga and Oswego
counties.
After a flurry of competitive maneuvering in 1997-1998 in anticipation of managed
care growth, the Syracuse health care market has settled into an uneasy calm,
as consolidation among local insurers has muted concerns that aggressive managed
care will take hold. Indeed, a series of health plan exits and mergers have left
indemnity insurer Excellus Blue Cross Blue Shield with about 40 percent of the
Syracuse market, which has produced a new stabilizing force in the local market.
Nevertheless, hospitals have struggled financially in face of reduced payment
rates, operational problems and long-term debt.
Other developments in Syracuse include the following:
- Under mounting financial pressure, the largest local
hospital system has filed for bankruptcy, while it and
others are taking steps to cut costs.
- Physicians are increasingly concerned about how they
will be affected by the growing clout of Excellus.
- New York State has continued to expand access to
health insurance and strengthen the local safety net.
Health Plan Shakeout Leaves One Dominant Indemnity Insurer
 ven the limited presence and influence
of managed care in the Syracuse market
appears to be diminishing. In a market
where hospital rate regulation and lack
of employer interest stymied the growth
of managed care products for many years,
Syracuse has long been a bastion of
indemnity insurance. Since 1998, plans
with tight managed care products have
downgraded their activities in Syracuse,
left the market entirely or been absorbed
by Excellus.
The most dramatic of these developments came in late 2000, when Excellus announced
plans to acquire Univera, the largest health maintenance organization (HMO) in
Syracuse, with 130,000 members. Univera was formed in the late 1990s from a merger
of HealthCarePlan of Buffalo and PHP, the latter a product of the national HMO
movement that began in the 1970s. The acquisition of Univera by Excellus will
bring an estimated 40 percent of the Syracuse market under one insurer.
Even before the Excellus-Univera deal
was announced, plan exits and reconfigurations
had reduced managed care options
in Syracuse. CIGNA withdrew its HMO
product from the market, remaining
largely to provide looser products to
major national accounts. Kaiser left the
Northeast altogether. North Medical
Community Health Plan, a local HMO
developed by a physician-entrepreneur,
sold out to Excellus because of increasing
financial difficulties. United Healthcare
consolidated its central New York operations
with those in New York City and
downgraded its Syracuse operations to a
submarket. And Aetna’s attempt to launch
an HMO product in this market has stalled,
reportedly because of the firm’s inability to
form an adequate provider network.
The Syracuse market appears to have
embraced consolidation among insurers
as an antidote to the competitive pressures that were unleashed in the aftermath
of New York State’s 1996 deregulation of
hospital rates. This transition from one
form of stability to another has been
relatively easy because of the regulatory heritage
in New York and the general antipathy
for outside, for-profit health plans.
Managed care penetration in the Syracuse market-including preferred provider organizations
(PPOs), which state laws had prohibited until the late 1990s-is now less than
40 percent. Moreover, the area’s moderate HMO enrollment has been migrating to
point-of- service (POS) and PPO products. Managed care’s weakness in Syracuse
is typified by the experience of Blue Cross Blue Shield of Central New York. This
Excellus subsidiary has grown approximately 20 percent since the Excellus acquisition
two years ago, mainly in its indemnity and PPO/POs products.
Neither purchasers nor consumers
have displayed much interest in HMOs
or other tight managed care products.
Unlike employers in nearby Rochester
and Buffalo that have long supported
community-rated HMOs, Syracuse
employers have favored open network
products and initiated few efforts to
influence either costs or quality in the
market. More than two-thirds of Excellus’
business is in its traditional indemnity
products, which have the advantages of a
broad network PPO, such as wide choice
and open access, and few disadvantages
from a consumer perspective. Moreover,
with considerable leverage over providers,
Excellus has displayed little interest in
downstreaming risk to promote managed
care incentives. ven the limited presence and influence
of managed care in the Syracuse market
appears to be diminishing. In a market
where hospital rate regulation and lack
of employer interest stymied the growth
of managed care products for many years,
Syracuse has long been a bastion of
indemnity insurance. Since 1998, plans
with tight managed care products have
downgraded their activities in Syracuse,
left the market entirely or been absorbed
by Excellus.
The most dramatic of these developments came in late 2000, when Excellus announced
plans to acquire Univera, the largest health maintenance organization (HMO) in
Syracuse, with 130,000 members. Univera was formed in the late 1990s from a merger
of HealthCarePlan of Buffalo and PHP, the latter a product of the national HMO
movement that began in the 1970s. The acquisition of Univera by Excellus will
bring an estimated 40 percent of the Syracuse market under one insurer.
Even before the Excellus-Univera deal
was announced, plan exits and reconfigurations
had reduced managed care options
in Syracuse. CIGNA withdrew its HMO
product from the market, remaining
largely to provide looser products to
major national accounts. Kaiser left the
Northeast altogether. North Medical
Community Health Plan, a local HMO
developed by a physician-entrepreneur,
sold out to Excellus because of increasing
financial difficulties. United Healthcare
consolidated its central New York operations
with those in New York City and
downgraded its Syracuse operations to a
submarket. And Aetna’s attempt to launch
an HMO product in this market has stalled,
reportedly because of the firm’s inability to
form an adequate provider network.
The Syracuse market appears to have
embraced consolidation among insurers
as an antidote to the competitive pressures that were unleashed in the aftermath
of New York State’s 1996 deregulation of
hospital rates. This transition from one
form of stability to another has been
relatively easy because of the regulatory heritage
in New York and the general antipathy
for outside, for-profit health plans.
Managed care penetration in the Syracuse market-including preferred provider organizations
(PPOs), which state laws had prohibited until the late 1990s-is now less than
40 percent. Moreover, the area’s moderate HMO enrollment has been migrating to
point-of- service (POS) and PPO products. Managed care’s weakness in Syracuse
is typified by the experience of Blue Cross Blue Shield of Central New York. This
Excellus subsidiary has grown approximately 20 percent since the Excellus acquisition
two years ago, mainly in its indemnity and PPO/POs products.
Neither purchasers nor consumers
have displayed much interest in HMOs
or other tight managed care products.
Unlike employers in nearby Rochester
and Buffalo that have long supported
community-rated HMOs, Syracuse
employers have favored open network
products and initiated few efforts to
influence either costs or quality in the
market. More than two-thirds of Excellus’
business is in its traditional indemnity
products, which have the advantages of a
broad network PPO, such as wide choice
and open access, and few disadvantages
from a consumer perspective. Moreover,
with considerable leverage over providers,
Excellus has displayed little interest in
downstreaming risk to promote managed
care incentives.
Hospitals Struggle Under Growing Financial Pressures
 he financial condition of Syracuse hospitals
has worsened over the past two
years, culminating with the February
2001 bankruptcy filing by the largest
hospital system. The 566-bed Crouse
Hospital filed for Chapter 11 bankruptcy
protection after facing declining payment
from both public and private payers and
more than $90 million in long-term debt.
The hospital had recently joined forces
with Community General Hospital in an
effort to gain operational efficiencies.
Under a parent holding company called
the Health Alliance of Central New York,
the two hospitals had embarked on a
number of cost-cutting initiatives to
address mounting losses at both facilities.
However, the two hospitals did not merge
assets and remain distinct facilities operating
under their original names, without
consolidating the clinical services offered
by each institution. Under its bankruptcy
protection request, Crouse Hospital
maintains that no services will be closed
and that patient care will go uninterrupted
during the restructuring. Rather, Crouse
views this action as necessary to obtain
relief from creditors while reorganizing
its finances.
Meanwhile, Syracuse’s other major hospitals also have experienced financial woes,
dampening their long-standing collaborative spirit as hospitals focus on improving
their bottom lines. Though area hospitals continue to work together on quality
and disease management issues through a collaborative group called the Hospital
Executive Council, these issues have become less pressing, while competitive pressures
have mounted. Fueled by the deregulation of hospital rates in 1996 and expectations
of growing HMO penetration and provider risk-sharing, Syracuse hospitals prepared
cautiously in 1997-1998 to negotiate competitive rates with health plans by cutting
costs and exploring alliances. Two years later, however, this activity has resulted
in little change in the structure of the local hospital market, and Syracuse hospitals
remain focused largely on internal operational issues.
Like Crouse and Community hospitals,
Syracuse’s two other major hospitals-
St. Joseph’s Hospital and University
Hospital-have not embarked on any
major initiatives to increase market
share, revenue or clout since 1998. Instead,
facing budget deficits and Medicare
payment reductions, the hospitals have
focused on cutting costs, reducing outpatient
services and programs and enhancing
inpatient clinical capacity in areas of historic
strength. St. Joseph’s, for example,
has cut operating costs in its outpatient
clinics, which serve many low-income
individuals, to keep the clinics open,
while University Hospital reduced staff
by 300 full-time equivalents (FTEs) over
the past few years, which helped it to
avoid red ink in 1999.
The effects of Medicare payment
cuts on Syracuse hospitals have been
exacerbated by a growing shortage of
nurses. All four hospitals have significant
nursing staff vacancies, which limit their
inpatient and outpatient capacity and
thus their ability to generate revenue.
An ongoing emergency room diversion
program-which directs ambulances to
a hospital with available inpatient beds-
has gained importance as hospitals’ ability
to staff units has eroded. This program
stands as an important remnant of
hospitals’ collaborative approach to
community health problems.
As in the past, there is some
sentiment among local observers that
Syracuse has too many hospitals-and
the Crouse/Community General alliance
has not dramatically changed the Syracuse
hospital environment in this regard.
Local observers disagree about whether
or when a hospital closure might actually
occur, and if it does, which hospital
would close.
Five smaller community hospitals
serve the suburban counties outside of
Syracuse. Neither these community hospitals
nor the four Syracuse hospitals have
sought formal alliances to shore up referral
networks or otherwise expand market
share the way hospitals in other markets
have. The reason may be that the suburban
hospitals are sole community providers
that have considerable bargaining clout
with insurers, and the city hospitals are
satisfied with the referrals and transfers
that they now receive from outside
Syracuse. he financial condition of Syracuse hospitals
has worsened over the past two
years, culminating with the February
2001 bankruptcy filing by the largest
hospital system. The 566-bed Crouse
Hospital filed for Chapter 11 bankruptcy
protection after facing declining payment
from both public and private payers and
more than $90 million in long-term debt.
The hospital had recently joined forces
with Community General Hospital in an
effort to gain operational efficiencies.
Under a parent holding company called
the Health Alliance of Central New York,
the two hospitals had embarked on a
number of cost-cutting initiatives to
address mounting losses at both facilities.
However, the two hospitals did not merge
assets and remain distinct facilities operating
under their original names, without
consolidating the clinical services offered
by each institution. Under its bankruptcy
protection request, Crouse Hospital
maintains that no services will be closed
and that patient care will go uninterrupted
during the restructuring. Rather, Crouse
views this action as necessary to obtain
relief from creditors while reorganizing
its finances.
Meanwhile, Syracuse’s other major hospitals also have experienced financial woes,
dampening their long-standing collaborative spirit as hospitals focus on improving
their bottom lines. Though area hospitals continue to work together on quality
and disease management issues through a collaborative group called the Hospital
Executive Council, these issues have become less pressing, while competitive pressures
have mounted. Fueled by the deregulation of hospital rates in 1996 and expectations
of growing HMO penetration and provider risk-sharing, Syracuse hospitals prepared
cautiously in 1997-1998 to negotiate competitive rates with health plans by cutting
costs and exploring alliances. Two years later, however, this activity has resulted
in little change in the structure of the local hospital market, and Syracuse hospitals
remain focused largely on internal operational issues.
Like Crouse and Community hospitals,
Syracuse’s two other major hospitals-
St. Joseph’s Hospital and University
Hospital-have not embarked on any
major initiatives to increase market
share, revenue or clout since 1998. Instead,
facing budget deficits and Medicare
payment reductions, the hospitals have
focused on cutting costs, reducing outpatient
services and programs and enhancing
inpatient clinical capacity in areas of historic
strength. St. Joseph’s, for example,
has cut operating costs in its outpatient
clinics, which serve many low-income
individuals, to keep the clinics open,
while University Hospital reduced staff
by 300 full-time equivalents (FTEs) over
the past few years, which helped it to
avoid red ink in 1999.
The effects of Medicare payment
cuts on Syracuse hospitals have been
exacerbated by a growing shortage of
nurses. All four hospitals have significant
nursing staff vacancies, which limit their
inpatient and outpatient capacity and
thus their ability to generate revenue.
An ongoing emergency room diversion
program-which directs ambulances to
a hospital with available inpatient beds-
has gained importance as hospitals’ ability
to staff units has eroded. This program
stands as an important remnant of
hospitals’ collaborative approach to
community health problems.
As in the past, there is some
sentiment among local observers that
Syracuse has too many hospitals-and
the Crouse/Community General alliance
has not dramatically changed the Syracuse
hospital environment in this regard.
Local observers disagree about whether
or when a hospital closure might actually
occur, and if it does, which hospital
would close.
Five smaller community hospitals
serve the suburban counties outside of
Syracuse. Neither these community hospitals
nor the four Syracuse hospitals have
sought formal alliances to shore up referral
networks or otherwise expand market
share the way hospitals in other markets
have. The reason may be that the suburban
hospitals are sole community providers
that have considerable bargaining clout
with insurers, and the city hospitals are
satisfied with the referrals and transfers
that they now receive from outside
Syracuse.
Physicians Cast about for Direction and Leverage
 any physicians have been left feeling
economically vulnerable in Syracuse’s
highly consolidated insurance market.
With the expectation of growing managed
care and competition, physicians formed
multispecialty independent practice associations
(IPAs) in the late 1990s, which
they hoped would give them more leverage
with health plans and hospitals.
However, over the past two years, one
IPA folded, and the two that remain have
struggled due to low HMO enrollment
and the fact that Excellus has not contracted
with IPAs. As these organizations
faltered, physicians have been left feeling
uneasy in a highly consolidated insurance
market-probably because provider payment
rates have not mirrored recent
insurance premium increases and, in
some cases, have been cut significantly.
Overall, Syracuse remains a market
dominated by solo or small-group physician
practices, and most physicians tend
to be affiliated with one of the four hospitals.
However, some consolidation has
occurred among single specialties. For
example, one group, Hematology-Oncology
Associates of Central New
York, has grown to 12 specialists, while
an orthopedics group, Syracuse Orthopedics
Specialists, is reported to have 17 orthopedists,
representing about 30 to 40
percent of the market. Cardiologists, on
the other hand, have not consolidated
and remain in many small practices
around the Syracuse area, unlike other
markets in which these specialists have
organized into large, powerful practices.
Formal physician-hospital integration
activities in Syracuse appear stagnant
or are faltering. Some hospitals have
reduced their ownership of primary care
practices and have de-emphasized other
arrangements that were expected to lead
to an integrated delivery system model.
Joint contracting with physicians is rare,
and although some hospitals provide
management services to affiliated physicians,
these services are not a major part
of overall market strategies. However, the
recent consolidation of insurers could
renew efforts to develop united negotiating
strategies among hospitals and their
affiliated physicians.
One area of competitive activity among physicians in Syracuse is the development
of ambulatory surgery centers (ASCs). In the wake of the relaxation of state certificate-of-need
rules, a number of physicians have invested in these centers to carve out a new
market niche. Hospitals view the growth of ASCs as a threat, potentially diverting
patients away from their own freestanding centers or outpatient departments. Health
plans, notably Excellus, have voiced concern about the potential for costly overcapacity. any physicians have been left feeling
economically vulnerable in Syracuse’s
highly consolidated insurance market.
With the expectation of growing managed
care and competition, physicians formed
multispecialty independent practice associations
(IPAs) in the late 1990s, which
they hoped would give them more leverage
with health plans and hospitals.
However, over the past two years, one
IPA folded, and the two that remain have
struggled due to low HMO enrollment
and the fact that Excellus has not contracted
with IPAs. As these organizations
faltered, physicians have been left feeling
uneasy in a highly consolidated insurance
market-probably because provider payment
rates have not mirrored recent
insurance premium increases and, in
some cases, have been cut significantly.
Overall, Syracuse remains a market
dominated by solo or small-group physician
practices, and most physicians tend
to be affiliated with one of the four hospitals.
However, some consolidation has
occurred among single specialties. For
example, one group, Hematology-Oncology
Associates of Central New
York, has grown to 12 specialists, while
an orthopedics group, Syracuse Orthopedics
Specialists, is reported to have 17 orthopedists,
representing about 30 to 40
percent of the market. Cardiologists, on
the other hand, have not consolidated
and remain in many small practices
around the Syracuse area, unlike other
markets in which these specialists have
organized into large, powerful practices.
Formal physician-hospital integration
activities in Syracuse appear stagnant
or are faltering. Some hospitals have
reduced their ownership of primary care
practices and have de-emphasized other
arrangements that were expected to lead
to an integrated delivery system model.
Joint contracting with physicians is rare,
and although some hospitals provide
management services to affiliated physicians,
these services are not a major part
of overall market strategies. However, the
recent consolidation of insurers could
renew efforts to develop united negotiating
strategies among hospitals and their
affiliated physicians.
One area of competitive activity among physicians in Syracuse is the development
of ambulatory surgery centers (ASCs). In the wake of the relaxation of state certificate-of-need
rules, a number of physicians have invested in these centers to carve out a new
market niche. Hospitals view the growth of ASCs as a threat, potentially diverting
patients away from their own freestanding centers or outpatient departments. Health
plans, notably Excellus, have voiced concern about the potential for costly overcapacity.
Employers Face Steep Premium Increases
 yracuse has enjoyed lower health insurance
premiums than many other markets,
but rates have increased by 15 percent for
two straight years, confronting employers
with rapidly rising costs. Purchaser resistance
to premium increases has been
muted, however, in part because of a
tight labor market, and in part because
Syracuse employers historically have not
taken an active role in shaping the local
health care system. Furthermore, efforts
to contain costs are less effective in an environment
in which hospitals have pushed
for and are now receiving rate increases
after a period of little or no growth.
Syracuse employers have shown little
interest in quality improvement initiatives
or other strategies that could help to shape
the market. Their preference appears to be
for their health plan or third-party administrator
to negotiate with providers and
ensure quality. Their reluctance to get
involved in the health care system is
attributable to a number of factors: a lack
of local leadership, because many large
employers are part of national corporations
with headquarters elsewhere; the dominance
of small, service-sector businesses;
and the influence of unions over the structure
and scope of employee health benefits.
Employers in Syracuse tend to offer indemnity plans or managed care products with
open networks, often PPO or POs products. HMOs’ rates were once comparable to
rates for these looser products, but some Syracuse employers report that recent
increases in HMO premiums have made HMOs more expensive. Employers have not yet
made major changes to benefit or cost-sharing structures in response to these
rate hikes, except in prescription drugs. Formularies were rare in this market
until 1998, but rising drug costs have led some employers to raise their prescription
copayments, move to a three-tier benefit structure or even mandate the use of
generic drugs. Some other employers have increased general cost-sharing amounts
from, for example, $5 per office visit to $10. yracuse has enjoyed lower health insurance
premiums than many other markets,
but rates have increased by 15 percent for
two straight years, confronting employers
with rapidly rising costs. Purchaser resistance
to premium increases has been
muted, however, in part because of a
tight labor market, and in part because
Syracuse employers historically have not
taken an active role in shaping the local
health care system. Furthermore, efforts
to contain costs are less effective in an environment
in which hospitals have pushed
for and are now receiving rate increases
after a period of little or no growth.
Syracuse employers have shown little
interest in quality improvement initiatives
or other strategies that could help to shape
the market. Their preference appears to be
for their health plan or third-party administrator
to negotiate with providers and
ensure quality. Their reluctance to get
involved in the health care system is
attributable to a number of factors: a lack
of local leadership, because many large
employers are part of national corporations
with headquarters elsewhere; the dominance
of small, service-sector businesses;
and the influence of unions over the structure
and scope of employee health benefits.
Employers in Syracuse tend to offer indemnity plans or managed care products with
open networks, often PPO or POs products. HMOs’ rates were once comparable to
rates for these looser products, but some Syracuse employers report that recent
increases in HMO premiums have made HMOs more expensive. Employers have not yet
made major changes to benefit or cost-sharing structures in response to these
rate hikes, except in prescription drugs. Formularies were rare in this market
until 1998, but rising drug costs have led some employers to raise their prescription
copayments, move to a three-tier benefit structure or even mandate the use of
generic drugs. Some other employers have increased general cost-sharing amounts
from, for example, $5 per office visit to $10.
State Shifts Regulatory Focus, Expands Coverage
 ew York State has continued its long-standing
support of programs that
expand access to health insurance and
strengthen the local safety net through
expansions of public insurance programs
and direct subsidies for charity care.
Efforts in Syracuse to enroll children and
adults in Medicaid and Child Health Plus,
New York’s State Children’s Health
Insurance Program (SCHIP), by and
large, have been innovative and successful.
The deregulation of hospital rates in 1996,
with subsequent increases in market
competition, has led to a new regulatory
emphasis: oversight of managed care.
Syracuse has mobilized an impressive
program of outreach and decentralized
enrollment for Medicaid managed care
and Child Health Plus, which preceded
the federal SCHIP program by several
years. Ironically, these efforts, which
include all four major hospitals, local
public health and many nontraditional
organizations-such as schools, churches
and community groups-have enrolled
many Medicaid-eligible children in Child
Health Plus. Now federal and state governments
are pushing hard to identify
and move these children out of Child
Health Plus into Medicaid, a situation
that has raised concern that children will
lose coverage and fall between the cracks.
Despite this challenge, implementation
of Child Health Plus and mandatory
Medicaid managed care in Onondaga and
Oswego counties, which started in 1999,
has gone smoothly. Four health plans,
including two commercial insurers
(Excellus and United) and two health plans
that serve only public clients (Total Care
and Fidelis), participate in both programs.
The safety net, comprising the
four Syracuse hospitals and Syracuse
Community Health Center (CHC), is
reasonably stable and expanding modestly
as a result of Child Health Plus and
Medicaid managed care. The funding
pools for charity care and graduate medical
education, which were created in 1996,
and expanded in 1998 as part of the Health
Care Reform Act (HCRA) of 2000, have
mitigated some of the effects that market
changes and dislocation might have had
on care for the uninsured. In addition,
Syracuse CHC has sought innovative program
expansions and revenue streams
more aggressively, and Total Care, its
affiliated health plan, is expanding into
at least two neighboring counties through
contracts with private clinics, a move that
will increase the region’s safety net capacity.
On the other hand, in an effort to
shore up their financial condition, hospitals
have had to cut services in outpatient
clinics used by uninsured patients.
HCRA 2000 established two new
programs designed to extend subsidized
health insurance coverage to additional
populations. Healthy New York began in
January 2001 to subsidize coverage in the
individual and small group markets
through reinsurance pools, which will
cover individuals’ medical costs above a
certain threshold and thus keep individual
and small group premiums lower. Family
Health Plus-slated to start in early 2001
pending federal approval-will expand
Medicaid eligibility to adults ages 19 to 64.
Governor George Pataki’s administration
has brought a strong emphasis on
nonregulatory solutions to health care
issues, starting with deregulation of
hospital rates. This marked shift in state
policy led to a short period of increased
competition and consolidation, but market
forces and the new focus on regulating
managed care have ended that phase.
The state departments of Insurance and
Health share-and, in some cases, compete
over-responsibility for overseeing
the activities of health plans and providers,
most notably the new external review
program and proposed regulations regarding
IPAs and risk-bearing provider organizations.
In addition, New York has invested
considerable resources in producing and
disseminating information about health
plans and providers to consumers and the
general public. Nonetheless, observers are
unclear about the objectives and outcomes
of these information initiatives. ew York State has continued its long-standing
support of programs that
expand access to health insurance and
strengthen the local safety net through
expansions of public insurance programs
and direct subsidies for charity care.
Efforts in Syracuse to enroll children and
adults in Medicaid and Child Health Plus,
New York’s State Children’s Health
Insurance Program (SCHIP), by and
large, have been innovative and successful.
The deregulation of hospital rates in 1996,
with subsequent increases in market
competition, has led to a new regulatory
emphasis: oversight of managed care.
Syracuse has mobilized an impressive
program of outreach and decentralized
enrollment for Medicaid managed care
and Child Health Plus, which preceded
the federal SCHIP program by several
years. Ironically, these efforts, which
include all four major hospitals, local
public health and many nontraditional
organizations-such as schools, churches
and community groups-have enrolled
many Medicaid-eligible children in Child
Health Plus. Now federal and state governments
are pushing hard to identify
and move these children out of Child
Health Plus into Medicaid, a situation
that has raised concern that children will
lose coverage and fall between the cracks.
Despite this challenge, implementation
of Child Health Plus and mandatory
Medicaid managed care in Onondaga and
Oswego counties, which started in 1999,
has gone smoothly. Four health plans,
including two commercial insurers
(Excellus and United) and two health plans
that serve only public clients (Total Care
and Fidelis), participate in both programs.
The safety net, comprising the
four Syracuse hospitals and Syracuse
Community Health Center (CHC), is
reasonably stable and expanding modestly
as a result of Child Health Plus and
Medicaid managed care. The funding
pools for charity care and graduate medical
education, which were created in 1996,
and expanded in 1998 as part of the Health
Care Reform Act (HCRA) of 2000, have
mitigated some of the effects that market
changes and dislocation might have had
on care for the uninsured. In addition,
Syracuse CHC has sought innovative program
expansions and revenue streams
more aggressively, and Total Care, its
affiliated health plan, is expanding into
at least two neighboring counties through
contracts with private clinics, a move that
will increase the region’s safety net capacity.
On the other hand, in an effort to
shore up their financial condition, hospitals
have had to cut services in outpatient
clinics used by uninsured patients.
HCRA 2000 established two new
programs designed to extend subsidized
health insurance coverage to additional
populations. Healthy New York began in
January 2001 to subsidize coverage in the
individual and small group markets
through reinsurance pools, which will
cover individuals’ medical costs above a
certain threshold and thus keep individual
and small group premiums lower. Family
Health Plus-slated to start in early 2001
pending federal approval-will expand
Medicaid eligibility to adults ages 19 to 64.
Governor George Pataki’s administration
has brought a strong emphasis on
nonregulatory solutions to health care
issues, starting with deregulation of
hospital rates. This marked shift in state
policy led to a short period of increased
competition and consolidation, but market
forces and the new focus on regulating
managed care have ended that phase.
The state departments of Insurance and
Health share-and, in some cases, compete
over-responsibility for overseeing
the activities of health plans and providers,
most notably the new external review
program and proposed regulations regarding
IPAs and risk-bearing provider organizations.
In addition, New York has invested
considerable resources in producing and
disseminating information about health
plans and providers to consumers and the
general public. Nonetheless, observers are
unclear about the objectives and outcomes
of these information initiatives.
Issues to Track
 nsurer consolidation has replaced hospital
regulation as the main stabilizing force
in Syracuse, a health care market that saw
considerable competitive activity for a
short period in 1997-1998. To cope with
rising premiums-due to both the insurance
underwriting cycle and the lack of
aggressive managed care-purchasers
have been content to adjust their benefit
packages on the margins rather than take
steps to shape the system as a whole.
Likewise, the area’s hospitals have not
undertaken major competitive initiatives
but have focused instead on near-term
efforts to reduce budget shortfalls. After
a brief flirtation with greater integration,
physicians are now concerned about the
power of payers, especially Excellus, to
determine their financial fates. Meanwhile,
New York State has continued its expansion
of public programs that increase
access to the uninsured and strengthen
the local safety net.
As the Syracuse market continues
to unfold, the following issues will be
important to track: nsurer consolidation has replaced hospital
regulation as the main stabilizing force
in Syracuse, a health care market that saw
considerable competitive activity for a
short period in 1997-1998. To cope with
rising premiums-due to both the insurance
underwriting cycle and the lack of
aggressive managed care-purchasers
have been content to adjust their benefit
packages on the margins rather than take
steps to shape the system as a whole.
Likewise, the area’s hospitals have not
undertaken major competitive initiatives
but have focused instead on near-term
efforts to reduce budget shortfalls. After
a brief flirtation with greater integration,
physicians are now concerned about the
power of payers, especially Excellus, to
determine their financial fates. Meanwhile,
New York State has continued its expansion
of public programs that increase
access to the uninsured and strengthen
the local safety net.
As the Syracuse market continues
to unfold, the following issues will be
important to track:
- What effects will the Excellus-Univera
merger have on consumers, provider
networks and relationships and other
health plans?
- Will continuing financial pressures force
any of Syracuse’s four hospitals to close?
- Will providers organize to increase their
market clout, so that they can demand
higher payment rates?
- How will employers cope with rising
health plan premiums for their
employees?
- Will New York’s new insurance expansions
continue the successes of the
Medicaid and Child Health Plus
programs?
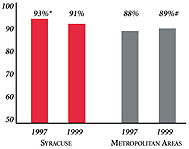
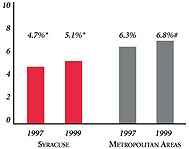
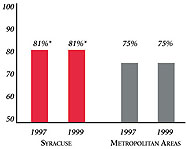
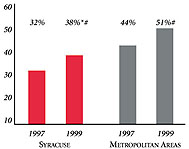
Syracuse’s Experience with the Local Health System, 1997 and 1999
Background and Observations
| Syracuse Demographics |
| Syracuse |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
732,920 |
| Population Change, 1990-19992
|
| -1.3% |
8.6% |
| Median Income3 |
| $24,619 |
$27,843 |
| Persons Living in Poverty3 |
| 14% |
14% |
| Persons Age 65 or Older3 |
| 14% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Syracuse |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 9.7% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 3.7% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 83% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $163 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Syracuse |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 2.9 |
2.8 |
| Physicians per 1,000 Population2
|
| 2.4 |
2.3 |
| HMO Penetration, 19973 |
| 19% |
32% |
| HMO Penetration, 19994 |
| 21% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Syracuse Community Report:
Aaron Katz, University of Washington
Robert E. Hurley, Virginia Commonwealth University
Leslie Jackson, HSC
Timothy K. Lake, Mathematica Policy Research
Ashley Short, HSC
James D. Reschovsky, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|