Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Hospitals Compete for Specialty Care
Greenville, S.C.
Community Report No. 07
Spring 2001
Glen P. Mays, Sally Trude, Lawrence P. Casalino, Patricia Lichiello, Bradley C. Strunk, Jeffrey Stoddard
 n November 2000, a team of
researchers visited Greenville, S.C., to
study that community’s health system,
how it is changing and the effects of
those changes on consumers. The
Center for Studying Health System
Change (HSC), as part of the
Community Tracking Study, interviewed
more than 50 leaders in the
health care market. Greenville is one of
12 communities tracked by HSC every
two years through site visits and surveys.
Individual community reports
are published for each round of site
visits. The first two site visits to
Greenville, in 1996 and 1998, provided
baseline and initial trend information
against which changes are tracked.
The Greenville market includes
Greenville, Spartanburg, Anderson,
Cherokee and Pickens counties. n November 2000, a team of
researchers visited Greenville, S.C., to
study that community’s health system,
how it is changing and the effects of
those changes on consumers. The
Center for Studying Health System
Change (HSC), as part of the
Community Tracking Study, interviewed
more than 50 leaders in the
health care market. Greenville is one of
12 communities tracked by HSC every
two years through site visits and surveys.
Individual community reports
are published for each round of site
visits. The first two site visits to
Greenville, in 1996 and 1998, provided
baseline and initial trend information
against which changes are tracked.
The Greenville market includes
Greenville, Spartanburg, Anderson,
Cherokee and Pickens counties.
Greenville’s continued population growth and economic
development have kept the area’s health care providers
busy and profitable. Hospitals have expanded specialty
services while abandoning efforts to build primary care
capacity. Health maintenance organization (HMO) enrollment
has remained low over the past two years, and distinctions
between HMOs and preferred provider organizations
(PPOs) have diminished. Rising insurance premiums
have prompted some small employers to drop coverage
for dependents, raising concerns about growth of the uninsured
population. Fortunately, access to care for under-served
populations has continued to improve through
cooperative efforts among safety net providers and other
community organizations.
Other significant developments over the past two years
include:
- Several area hospitals have received state approval to
offer tertiary care services, leading to more intense
competition for patients.
- Providers have discontinued efforts to build infrastructure
for managed care risk contracting.
- Projected state budget shortfalls have begun to threaten
the long-term stability of government health insurance
programs, including Medicaid and the State Children’s
Health Insurance Program (SCHIP).
Competition Intensifies as Hospitals Strengthen Specialty Care
 reenville’s hospital systems have remained financially sound
and powerful in the local market over the past two years. Steady population growth
has kept most hospitals operating at full capacity, strengthening their negotiating
leverage with health plans and physicians. After a failed merger attempt among
three of the region’s largest hospital systems in 1996, hospitals have concentrated
on relatively distinct submarkets generally defined by the municipal boundaries
of Greenville, Spartanburg and Anderson. Historically, the competition for patients
across these submarkets has been fairly limited, and Greenville Hospital System
(GHS) has been the dominant local provider of tertiary care and other specialty
services.
Since 1998, however, most area
hospitals have strengthened their ability
to deliver profitable specialty services such
as cardiology, oncology and orthopedics.
Consequently, hospitals have begun to
compete more aggressively for patients
and revenue in these services. Spartanburg
Regional Healthcare System, for example,
built a new cancer center and increased
its capacity to perform cardiac surgery.
Spartanburg’s other major hospital, Mary
Black Memorial Hospital, recently formed
an alliance with a national oncology service
provider to expand the hospital’s cancer
services. Similarly, Anderson Area Medical
Center received state approval to open a
cardiac surgery center.
During this same period, Greenville’s
Bon Secours St. Francis Hospital opened
new cardiac surgery and bone marrow
transplantation centers and received state
approval to provide an expanded array of
neonatal intensive care services. These new
services were expected to improve the hospital’s
competitive position relative to the
nearby GHS, which has continued to offer
deep discounts to health insurers that
exclude St. Francis from their networks.
These exclusive contracts have remained in
place despite the expanded array of services
available at St. Francis, helping GHS to
retain its dominant position in the market.
Historically, state certificate-of-need
(CON) regulations have restricted competition
in the provision of tertiary care
services such as cardiac surgery and oncology,
but the area’s steady population growth
has prompted the state to approve recent
hospital requests to expand service offerings.
There has been little evidence to suggest
that recent service expansions have resulted
in unnecessary duplication and excess
capacity, as some local employers and
health plans feared. To the contrary, many
observers expected the recent expansions to
help alleviate emerging capacity constraints
caused by the region’s population growth. reenville’s hospital systems have remained financially sound
and powerful in the local market over the past two years. Steady population growth
has kept most hospitals operating at full capacity, strengthening their negotiating
leverage with health plans and physicians. After a failed merger attempt among
three of the region’s largest hospital systems in 1996, hospitals have concentrated
on relatively distinct submarkets generally defined by the municipal boundaries
of Greenville, Spartanburg and Anderson. Historically, the competition for patients
across these submarkets has been fairly limited, and Greenville Hospital System
(GHS) has been the dominant local provider of tertiary care and other specialty
services.
Since 1998, however, most area
hospitals have strengthened their ability
to deliver profitable specialty services such
as cardiology, oncology and orthopedics.
Consequently, hospitals have begun to
compete more aggressively for patients
and revenue in these services. Spartanburg
Regional Healthcare System, for example,
built a new cancer center and increased
its capacity to perform cardiac surgery.
Spartanburg’s other major hospital, Mary
Black Memorial Hospital, recently formed
an alliance with a national oncology service
provider to expand the hospital’s cancer
services. Similarly, Anderson Area Medical
Center received state approval to open a
cardiac surgery center.
During this same period, Greenville’s
Bon Secours St. Francis Hospital opened
new cardiac surgery and bone marrow
transplantation centers and received state
approval to provide an expanded array of
neonatal intensive care services. These new
services were expected to improve the hospital’s
competitive position relative to the
nearby GHS, which has continued to offer
deep discounts to health insurers that
exclude St. Francis from their networks.
These exclusive contracts have remained in
place despite the expanded array of services
available at St. Francis, helping GHS to
retain its dominant position in the market.
Historically, state certificate-of-need
(CON) regulations have restricted competition
in the provision of tertiary care
services such as cardiac surgery and oncology,
but the area’s steady population growth
has prompted the state to approve recent
hospital requests to expand service offerings.
There has been little evidence to suggest
that recent service expansions have resulted
in unnecessary duplication and excess
capacity, as some local employers and
health plans feared. To the contrary, many
observers expected the recent expansions to
help alleviate emerging capacity constraints
caused by the region’s population growth.
Providers Discontinue Preparations for Managed Care
 hile expanding specialty services, Greenville-area providers
have discontinued efforts to prepare for risk contracting with health plans. Before
1999, most hospitals in Greenville were actively purchasing primary care practices
across the region and investing in care management and quality-improvement initiatives-activities
that were designed to help hospitals attract and manage risk contracts with health
plans. Providers that experimented with risk contracting, however, found these
arrangements to be unprofitable given the area’s limited HMO enrollment, low capitation
payments and the high overhead costs associated with managing these contracts.
Consequently, most providers have lost all interest in risk contracting. For similar
reasons, Greenville’s only provider-sponsored health plan, HealthFirst, was dissolved
by its three hospital owners at the end of 1999 after only two years of operation.
Because risk contracting failed to
develop, hospitals have slowed their drive to
acquire primary care capacity over the past
two years. Moreover, some hospitals have
scaled back efforts to develop care management
initiatives designed to reduce utilization
and improve service delivery. In 1998,
several of Greenville’s leading hospital systems
had begun to develop and implement
such initiatives for complex and high-cost
medical conditions. According to hospital
administrators, some of these programs
could not be sustained financially because
health plan contracts did not reward hospital
efforts to prevent readmissions and
improve outpatient recovery. A few care
management initiatives have continued to
operate in hospitals-such as Spartanburg
Regional Healthcare System’s programs for
congestive heart failure and diabetes-but
efforts to expand these programs to new
disease areas have been suspended. Some
community leaders have become concerned
that local providers no longer face significant
external pressures to improve the
quality and efficiency of clinical practice. hile expanding specialty services, Greenville-area providers
have discontinued efforts to prepare for risk contracting with health plans. Before
1999, most hospitals in Greenville were actively purchasing primary care practices
across the region and investing in care management and quality-improvement initiatives-activities
that were designed to help hospitals attract and manage risk contracts with health
plans. Providers that experimented with risk contracting, however, found these
arrangements to be unprofitable given the area’s limited HMO enrollment, low capitation
payments and the high overhead costs associated with managing these contracts.
Consequently, most providers have lost all interest in risk contracting. For similar
reasons, Greenville’s only provider-sponsored health plan, HealthFirst, was dissolved
by its three hospital owners at the end of 1999 after only two years of operation.
Because risk contracting failed to
develop, hospitals have slowed their drive to
acquire primary care capacity over the past
two years. Moreover, some hospitals have
scaled back efforts to develop care management
initiatives designed to reduce utilization
and improve service delivery. In 1998,
several of Greenville’s leading hospital systems
had begun to develop and implement
such initiatives for complex and high-cost
medical conditions. According to hospital
administrators, some of these programs
could not be sustained financially because
health plan contracts did not reward hospital
efforts to prevent readmissions and
improve outpatient recovery. A few care
management initiatives have continued to
operate in hospitals-such as Spartanburg
Regional Healthcare System’s programs for
congestive heart failure and diabetes-but
efforts to expand these programs to new
disease areas have been suspended. Some
community leaders have become concerned
that local providers no longer face significant
external pressures to improve the
quality and efficiency of clinical practice.
Physician-Hospital Relationships Remain Strong
 hysicians have remained tightly aligned
with Greenville-area hospitals, despite the
hospitals’ waning interest in building primary
care capacity. During the mid-1990s,
hospitals pursued close relationships with
physicians to prepare for risk contracting,
either through physician-hospital organizations
(PHOs) or by acquiring physician
practices. By 1997, nearly 75 percent of
Greenville’s primary care physicians were
employed by hospitals, and most hospitals
had developed active PHOs. Though no
longer focused on risk contracting, many
of these arrangements have remained intact
and have become important vehicles for exercising
negotiating leverage with health plans.
Indeed, most Greenville-area hospitals
have succeeded in negotiating substantial
payment increases from health plans over
the past two years, and plans have attributed
these successes in part to the tight alignment
between physicians and hospitals. For example,
GHS has continued to employ nearly
180 physicians in both primary care and
specialty disciplines, helping the system to
remain an indispensable provider in health
plan networks. Similarly, Spartanburg
Regional Healthcare System’s PHO, Regional
HealthPlus, has become an important vehicle
for both HMO and PPO contracting.
Because the hospital and its participating
physicians share financial risk through a
withhold arrangement, the PHO reportedly
is able to negotiate fee-for-service
payment rates collectively on behalf of
the participating providers without raising
antitrust concerns.
To date, the only Greenville-area hospital
that has decided to sell its physician
practices is St. Francis. This hospital has
not been successful in using its 20 primary
care practices and 75 employed physicians
to gain negotiating leverage with health
plans, largely because two of the state’s
largest plans exclude it from their networks
to obtain discounts from GHS.
Physicians have found few nonhospital-based
strategies for exerting their leverage
collectively in the Greenville market.
Large independent physician groups have
remained absent from the Greenville area
since the demise of Carolina Multispecialty
Associates (CMA) at the end of 1998. CMA
had been organized several years earlier to
participate in risk contracts with health
plans, but its administrative infrastructure
proved too costly to sustain once these contracts
failed to develop in the market. With
CMA’s demise, several small single-specialty
groups have gained negotiating leverage
with plans and hospitals because of their
local dominance in specific lines of service.
Some of these single-specialty groups
have developed independent outpatient
surgery and imaging facilities that potentially
could compete with hospital-based
services, but so far these ventures have
remained limited in scope and scale.
Greenville-area hospitals generally have
been successful in using the state’s CON
regulations to block competition from free-standing
facilities. However, hospital administrators
expressed concern that proposed
changes to the state’s CON regulations could
allow more of these facilities to develop,
ultimately compromising the financial
viability of hospitals by stripping away
profitable specialty service lines. hysicians have remained tightly aligned
with Greenville-area hospitals, despite the
hospitals’ waning interest in building primary
care capacity. During the mid-1990s,
hospitals pursued close relationships with
physicians to prepare for risk contracting,
either through physician-hospital organizations
(PHOs) or by acquiring physician
practices. By 1997, nearly 75 percent of
Greenville’s primary care physicians were
employed by hospitals, and most hospitals
had developed active PHOs. Though no
longer focused on risk contracting, many
of these arrangements have remained intact
and have become important vehicles for exercising
negotiating leverage with health plans.
Indeed, most Greenville-area hospitals
have succeeded in negotiating substantial
payment increases from health plans over
the past two years, and plans have attributed
these successes in part to the tight alignment
between physicians and hospitals. For example,
GHS has continued to employ nearly
180 physicians in both primary care and
specialty disciplines, helping the system to
remain an indispensable provider in health
plan networks. Similarly, Spartanburg
Regional Healthcare System’s PHO, Regional
HealthPlus, has become an important vehicle
for both HMO and PPO contracting.
Because the hospital and its participating
physicians share financial risk through a
withhold arrangement, the PHO reportedly
is able to negotiate fee-for-service
payment rates collectively on behalf of
the participating providers without raising
antitrust concerns.
To date, the only Greenville-area hospital
that has decided to sell its physician
practices is St. Francis. This hospital has
not been successful in using its 20 primary
care practices and 75 employed physicians
to gain negotiating leverage with health
plans, largely because two of the state’s
largest plans exclude it from their networks
to obtain discounts from GHS.
Physicians have found few nonhospital-based
strategies for exerting their leverage
collectively in the Greenville market.
Large independent physician groups have
remained absent from the Greenville area
since the demise of Carolina Multispecialty
Associates (CMA) at the end of 1998. CMA
had been organized several years earlier to
participate in risk contracts with health
plans, but its administrative infrastructure
proved too costly to sustain once these contracts
failed to develop in the market. With
CMA’s demise, several small single-specialty
groups have gained negotiating leverage
with plans and hospitals because of their
local dominance in specific lines of service.
Some of these single-specialty groups
have developed independent outpatient
surgery and imaging facilities that potentially
could compete with hospital-based
services, but so far these ventures have
remained limited in scope and scale.
Greenville-area hospitals generally have
been successful in using the state’s CON
regulations to block competition from free-standing
facilities. However, hospital administrators
expressed concern that proposed
changes to the state’s CON regulations could
allow more of these facilities to develop,
ultimately compromising the financial
viability of hospitals by stripping away
profitable specialty service lines.
HMOs Fail to Gain Ground
 MOs have not gained substantial market share in Greenville’s
PPO-dominated health insurance market over the past two years. Blue Cross Blue
Shield of South Carolina has remained the dominant insurer, with approximately
40 percent of the commercial market, largely because of the popularity of its
PPO. One reason that HMOs have not grown as expected is that they have been unable
to offer purchasers and consumers substantial cost savings over PPOs. Health plan
administrators indicated that their short-lived experiments with risk contracting
were not effective in containing HMO costs because many of the area’s high-cost
providers declined to participate in such contracts. Moreover, because HMO enrollment
and physician supply have remained low in this market, many providers have become
unwilling to offer larger discounts to HMO products than to PPO products. As a
result, premiums for HMOs have risen sharply over the past two years and have
become comparable to PPO premiums.
In an effort to attract additional HMO
membership, several health plans have introduced
new direct-access HMO products
that do not require referrals for specialty
care. Three of Greenville’s largest insurance
carriers have launched some variant of
this product over the past year, largely in
response to the success that one plan experienced
with its direct-access HMO during
1998 and 1999. That success has contributed
to a modest growth in HMO enrollment
over the past two years-from 11 percent
of individuals with private insurance in 1998
to 14 percent in 2000. The emergence of
direct-access products, however, has blurred
the distinction between HMO and PPO
products. Benefits, product features and
premiums have become remarkably similar
across these once-distinct product lines.
As HMOs and PPOs have converged
in product design, HMOs have ceased to
function as low-cost health insurance
options for small businesses and other
purchasers challenged by rising premiums.
In response, several plans have stepped up
marketing of lower-priced HMO and PPO
products that have higher deductibles and
coinsurance levels for enrollees or that use
partial self-insurance arrangements that
require employers to cover a greater share
of health care costs. Examples include
products that require enrollees to pay 30
percent or more of each claim, and minimum
premium products that require
purchasers to pay all claims below an established
amount. Some observers expressed
concern that these types of products could
leave consumers and small businesses with
inadequate insurance benefits, while others
believed that few employers would purchase
such products. MOs have not gained substantial market share in Greenville’s
PPO-dominated health insurance market over the past two years. Blue Cross Blue
Shield of South Carolina has remained the dominant insurer, with approximately
40 percent of the commercial market, largely because of the popularity of its
PPO. One reason that HMOs have not grown as expected is that they have been unable
to offer purchasers and consumers substantial cost savings over PPOs. Health plan
administrators indicated that their short-lived experiments with risk contracting
were not effective in containing HMO costs because many of the area’s high-cost
providers declined to participate in such contracts. Moreover, because HMO enrollment
and physician supply have remained low in this market, many providers have become
unwilling to offer larger discounts to HMO products than to PPO products. As a
result, premiums for HMOs have risen sharply over the past two years and have
become comparable to PPO premiums.
In an effort to attract additional HMO
membership, several health plans have introduced
new direct-access HMO products
that do not require referrals for specialty
care. Three of Greenville’s largest insurance
carriers have launched some variant of
this product over the past year, largely in
response to the success that one plan experienced
with its direct-access HMO during
1998 and 1999. That success has contributed
to a modest growth in HMO enrollment
over the past two years-from 11 percent
of individuals with private insurance in 1998
to 14 percent in 2000. The emergence of
direct-access products, however, has blurred
the distinction between HMO and PPO
products. Benefits, product features and
premiums have become remarkably similar
across these once-distinct product lines.
As HMOs and PPOs have converged
in product design, HMOs have ceased to
function as low-cost health insurance
options for small businesses and other
purchasers challenged by rising premiums.
In response, several plans have stepped up
marketing of lower-priced HMO and PPO
products that have higher deductibles and
coinsurance levels for enrollees or that use
partial self-insurance arrangements that
require employers to cover a greater share
of health care costs. Examples include
products that require enrollees to pay 30
percent or more of each claim, and minimum
premium products that require
purchasers to pay all claims below an established
amount. Some observers expressed
concern that these types of products could
leave consumers and small businesses with
inadequate insurance benefits, while others
believed that few employers would purchase
such products.
Small Businesses Struggle with Escalating Premiums
 irroring national trends, employers in the Greenville market
have experienced significant premium increases over the past two years. Large
employers have not responded to the premium increases with major changes in their
health benefits programs as yet. Small employers, however, have faced more extreme
premium increases than their larger counterparts, and some have begun to drop
coverage for their employees’ dependents.
Many community leaders expressed
concern about the rapid decline in the
number of insurance carriers offering
affordable products to small businesses.
Although six carriers offer health insurance
products to businesses with fewer than 50
employees, employers considered only
three of these products to be affordable.
Insurance carriers have incurred large
financial losses in the small group business
line in the past two years, and 17 plans have
withdrawn from the state’s small group
market since mid-1997. Many respondents
blamed the 1996 federal Health
Insurance Portability and Accountability
Act (HIPAA) for considerable turmoil in
the small group market. However, the fact
that 46 insurers remain in this market
statewide suggests that exits were precipitated
in part by an overcrowded market.
The Greater Greenville Chamber of
Commerce and the newly formed Business
Council of South Carolina are each taking
steps to gain relief for small businesses in
purchasing health insurance. The Chamber
of Commerce is working to amend state
laws that limit businesses’ ability to develop
associations that enhance purchasing
power in the insurance market. In particular,
it seeks legislation to allow small
business associations to pool risk under a
single contract with insurance carriers, create
risk tiers for different types of association
members and design and purchase customized
health insurance products.
In a separate effort, the Business
Council of South Carolina is attempting
to increase membership in its newly
formed purchasing association. Additionally,
the organization is encouraging state officials
to develop a high-risk insurance pool
demonstration program that would provide
state-subsidized coverage for small
businesses unable to obtain coverage in
the private market because of their high
claims experience. It is unclear whether
this program will go beyond the proposal
stage, however, because of growing state
budget pressures. irroring national trends, employers in the Greenville market
have experienced significant premium increases over the past two years. Large
employers have not responded to the premium increases with major changes in their
health benefits programs as yet. Small employers, however, have faced more extreme
premium increases than their larger counterparts, and some have begun to drop
coverage for their employees’ dependents.
Many community leaders expressed
concern about the rapid decline in the
number of insurance carriers offering
affordable products to small businesses.
Although six carriers offer health insurance
products to businesses with fewer than 50
employees, employers considered only
three of these products to be affordable.
Insurance carriers have incurred large
financial losses in the small group business
line in the past two years, and 17 plans have
withdrawn from the state’s small group
market since mid-1997. Many respondents
blamed the 1996 federal Health
Insurance Portability and Accountability
Act (HIPAA) for considerable turmoil in
the small group market. However, the fact
that 46 insurers remain in this market
statewide suggests that exits were precipitated
in part by an overcrowded market.
The Greater Greenville Chamber of
Commerce and the newly formed Business
Council of South Carolina are each taking
steps to gain relief for small businesses in
purchasing health insurance. The Chamber
of Commerce is working to amend state
laws that limit businesses’ ability to develop
associations that enhance purchasing
power in the insurance market. In particular,
it seeks legislation to allow small
business associations to pool risk under a
single contract with insurance carriers, create
risk tiers for different types of association
members and design and purchase customized
health insurance products.
In a separate effort, the Business
Council of South Carolina is attempting
to increase membership in its newly
formed purchasing association. Additionally,
the organization is encouraging state officials
to develop a high-risk insurance pool
demonstration program that would provide
state-subsidized coverage for small
businesses unable to obtain coverage in
the private market because of their high
claims experience. It is unclear whether
this program will go beyond the proposal
stage, however, because of growing state
budget pressures.
Community Mobilizes Support for Expanding Safety Net
 he Greenville community has continued to expand access to
care for underserved populations through partnerships among safety net providers
and other community organizations. After significant gaps were identified four
years ago, the United Way organized a community-wide needs assessment that found
that more than 10 percent of residents were uninsured, and another 20 percent
were underinsured or otherwise medically underserved. The assessment triggered
several capital improvement efforts to expand local capacity to care for individuals
who lack access to medical care providers. Greenville’s two community health clinics
renovated their facilities and expanded clinical services, and several Greenville-area
hospitals committed funds to provide ongoing support for these improvements.
Efforts to expand the capacity of
Greenville’s safety net have continued
over the past two years, with a special
focus on coordinated, community-wide
efforts to improve access to care. As an
outgrowth of the 1997 assessment process,
local organizations formed the Community
Health Alliance (CHA) in 1999 to bring
together a broad range of organizations
interested in improving access to health
care, including health, civic, business and
faith-based organizations. The CHA has
coordinated efforts to develop satellite
community clinics in areas underserved
by medical care providers. It is also working
to increase the amount of charity care
delivered by local physicians, in part by
establishing a community-wide database
to recognize and monitor physician charity
care. Most recently, the CHA has undertaken
a study of the health insurance
benefits offered by small businesses in
hopes of designing a local program to
provide coverage to the uninsured
employees of these businesses.
Despite recent successes, safety net
providers remain concerned about access
to care for the uninsured and underserved.
Inadequate public transportation has
continued to pose barriers to health care
for many low-income Greenville County
residents. In 1996, the Greenville Transit
Authority was forced to reduce hours
and service areas because of funding
shortfalls. Community organizations
subsequently pieced together a medical
transportation network using public and
private funding, but local policy makers
have failed to adopt a permanent solution
to Greenville’s transportation problems.
At the same time, rising health insurance
premiums have raised fears among safety
net providers that private insurance coverage
has begun to erode and threatens to
overwhelm the community’s recent successes
in expanding care for the underserved. he Greenville community has continued to expand access to
care for underserved populations through partnerships among safety net providers
and other community organizations. After significant gaps were identified four
years ago, the United Way organized a community-wide needs assessment that found
that more than 10 percent of residents were uninsured, and another 20 percent
were underinsured or otherwise medically underserved. The assessment triggered
several capital improvement efforts to expand local capacity to care for individuals
who lack access to medical care providers. Greenville’s two community health clinics
renovated their facilities and expanded clinical services, and several Greenville-area
hospitals committed funds to provide ongoing support for these improvements.
Efforts to expand the capacity of
Greenville’s safety net have continued
over the past two years, with a special
focus on coordinated, community-wide
efforts to improve access to care. As an
outgrowth of the 1997 assessment process,
local organizations formed the Community
Health Alliance (CHA) in 1999 to bring
together a broad range of organizations
interested in improving access to health
care, including health, civic, business and
faith-based organizations. The CHA has
coordinated efforts to develop satellite
community clinics in areas underserved
by medical care providers. It is also working
to increase the amount of charity care
delivered by local physicians, in part by
establishing a community-wide database
to recognize and monitor physician charity
care. Most recently, the CHA has undertaken
a study of the health insurance
benefits offered by small businesses in
hopes of designing a local program to
provide coverage to the uninsured
employees of these businesses.
Despite recent successes, safety net
providers remain concerned about access
to care for the uninsured and underserved.
Inadequate public transportation has
continued to pose barriers to health care
for many low-income Greenville County
residents. In 1996, the Greenville Transit
Authority was forced to reduce hours
and service areas because of funding
shortfalls. Community organizations
subsequently pieced together a medical
transportation network using public and
private funding, but local policy makers
have failed to adopt a permanent solution
to Greenville’s transportation problems.
At the same time, rising health insurance
premiums have raised fears among safety
net providers that private insurance coverage
has begun to erode and threatens to
overwhelm the community’s recent successes
in expanding care for the underserved.
Medicaid Program Faces State Budget Pressures
 ecent expansions in state health care programs have bolstered
insurance coverage in Greenville and statewide, but a looming state budget crisis
in South Carolina has created uncertainty about the sustainability of these expansions.
In 1997, South Carolina’s Medicaid/SCHIP expansion for children, Partners for
Healthy Children, which covers children in households with incomes up to 150 percent
of the federal poverty level, brought in nearly 150,000 new Medicaid/SCHIP enrollees
statewide- almost twice the number that had been expected. As a result of this
new enrollment and other recent expansions in Medicaid benefits and coverage,
the state’s Medicaid expenses exceeded its year 2000 budget.
As a stopgap measure, South Carolina
used funds from its settlement with the
tobacco industry and other nonrecurring
state funds to address the budget shortfall.
However, this funding will not be available
to meet the state’s financial obligations in
subsequent years. As a result, the state faces
a Medicaid funding deficit that could reach
$300 million in 2001.
Despite the threat of a state health
care financing crisis, South Carolina’s
policy makers have remained cool toward
health care cost-containment strategies that
rely on managed care. The state has chosen
not to implement a program of mandatory
HMO enrollment for Medicaid recipients,
and it has allowed enrollment in its voluntary
Medicaid managed care program to
remain low over the past four years.
Statewide, only one plan currently participates
in the voluntary program, and most
Medicaid recipients have chosen to remain
in one of the program’s enhanced fee-for-service
options. The Greenville area has
been without a Medicaid HMO since the
now-defunct HealthFirst plan discontinued
Medicaid participation in 1998.
South Carolina’s Medicaid program
has continued to struggle with low levels of
private physician participation-a problem
that could be exacerbated if the state’s budget shortfall leads to Medicaid payment
cuts. Fee-for-service physician payments
under Medicaid have remained low, discouraging
physician participation in a
community already underserved by private
physicians. Greenville’s safety net providers,
therefore, have remained primary sources
of care, not only for uninsured populations,
but also for those covered by
Medicaid. Consequently, the state’s looming
budget crisis has generated concerns
about the financial stability of Greenville’s
safety net providers. ecent expansions in state health care programs have bolstered
insurance coverage in Greenville and statewide, but a looming state budget crisis
in South Carolina has created uncertainty about the sustainability of these expansions.
In 1997, South Carolina’s Medicaid/SCHIP expansion for children, Partners for
Healthy Children, which covers children in households with incomes up to 150 percent
of the federal poverty level, brought in nearly 150,000 new Medicaid/SCHIP enrollees
statewide- almost twice the number that had been expected. As a result of this
new enrollment and other recent expansions in Medicaid benefits and coverage,
the state’s Medicaid expenses exceeded its year 2000 budget.
As a stopgap measure, South Carolina
used funds from its settlement with the
tobacco industry and other nonrecurring
state funds to address the budget shortfall.
However, this funding will not be available
to meet the state’s financial obligations in
subsequent years. As a result, the state faces
a Medicaid funding deficit that could reach
$300 million in 2001.
Despite the threat of a state health
care financing crisis, South Carolina’s
policy makers have remained cool toward
health care cost-containment strategies that
rely on managed care. The state has chosen
not to implement a program of mandatory
HMO enrollment for Medicaid recipients,
and it has allowed enrollment in its voluntary
Medicaid managed care program to
remain low over the past four years.
Statewide, only one plan currently participates
in the voluntary program, and most
Medicaid recipients have chosen to remain
in one of the program’s enhanced fee-for-service
options. The Greenville area has
been without a Medicaid HMO since the
now-defunct HealthFirst plan discontinued
Medicaid participation in 1998.
South Carolina’s Medicaid program
has continued to struggle with low levels of
private physician participation-a problem
that could be exacerbated if the state’s budget shortfall leads to Medicaid payment
cuts. Fee-for-service physician payments
under Medicaid have remained low, discouraging
physician participation in a
community already underserved by private
physicians. Greenville’s safety net providers,
therefore, have remained primary sources
of care, not only for uninsured populations,
but also for those covered by
Medicaid. Consequently, the state’s looming
budget crisis has generated concerns
about the financial stability of Greenville’s
safety net providers.
Issues to Track
 reenville’s hospitals have strengthened specialty services
over the past two years, while safety net providers have expanded capacity to
provide care for the uninsured and other underserved populations. Rising health
care costs, however, have threatened to erode private health insurance coverage
at a time when South Carolina’s publicly funded insurance programs face substantial
budget shortfalls. These developments raise new questions about how health care
delivery and access to care in Greenville may change in the future: reenville’s hospitals have strengthened specialty services
over the past two years, while safety net providers have expanded capacity to
provide care for the uninsured and other underserved populations. Rising health
care costs, however, have threatened to erode private health insurance coverage
at a time when South Carolina’s publicly funded insurance programs face substantial
budget shortfalls. These developments raise new questions about how health care
delivery and access to care in Greenville may change in the future:
- Will safety net providers be able to meet the needs of the area’s uninsured
and publicly insured-given booming population growth and the expected erosion
of small businesses’ provision of health insurance?
- How will growing hospital competition
for specialty services affect health care
costs, quality and access?
- Will efforts to develop health insurance purchasing associations be successful
in containing premiums and improving insurance coverage among small businesses?
- How will state budget pressures affect eligibility, benefits and provider
payments under the state’s Medicaid and SCHIP expansion programs?
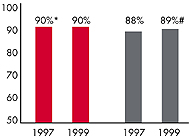
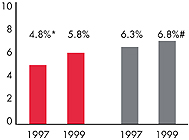
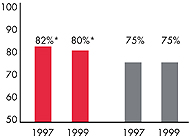
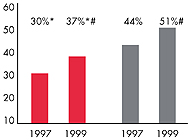
Greenville’s Experience with the Local Health System, 1997
and 1999
Background and Observations
| Greenville Demographics |
| Greenville |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
929,565 |
| Population Change, 1990-19992
|
| 12% |
8.6% |
| Median Income3 |
| $24,967 |
$27,843 |
| Persons Living in Poverty3 |
| 14% |
14% |
| Persons Age 65 or Older3 |
| 13% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Greenville |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 13% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 9% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 88% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $158 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Greenville |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 2.8 |
2.8 |
| Physicians per 1,000 Population2
|
| 1.7 |
2.3 |
| HMO Penetration, 19973 |
| 8.4% |
32% |
| HMO Penetration, 19994 |
| 13% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Greenville Community Report:
Glen P. Mays, Mathematica Policy Research, Inc.
Sally Trude, HSC
Lawrence P. Casalino, University of Chicago
Patricia Lichiello, University of Washington
Bradley C. Strunk, HSC
Jeffrey J. Stoddard, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|