Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Hopes Dim for More Competition
Little Rock, Ark.
Community Report No. 08
Spring 2001
Debra A. Draper, Linda R. Brewster, Lawrence D. Brown, Lance Heineccius, Carolyn A. Watts, Laurie E. Felland, Elizabeth Eagan
 n December 2000, a team of researchers visited Little Rock,
Ark., to study that community’s health system, how it is changing and the effects
of those changes on consumers. The Center for Studying Health System Change (HSC),
as part of the Community Tracking Study, interviewed more than 50 leaders in the
health care market. Little Rock is one of 12 communities tracked by HSC every
two years through site visits and surveys. Individual community reports are published
for each round of site visits. The first two site visits to Little Rock, in 1996
and 1998, provided baseline and initial trend information against which changes
are tracked. The Little Rock market includes Faulkner, Lonoke, Pulaski and Saline
counties. n December 2000, a team of researchers visited Little Rock,
Ark., to study that community’s health system, how it is changing and the effects
of those changes on consumers. The Center for Studying Health System Change (HSC),
as part of the Community Tracking Study, interviewed more than 50 leaders in the
health care market. Little Rock is one of 12 communities tracked by HSC every
two years through site visits and surveys. Individual community reports are published
for each round of site visits. The first two site visits to Little Rock, in 1996
and 1998, provided baseline and initial trend information against which changes
are tracked. The Little Rock market includes Faulkner, Lonoke, Pulaski and Saline
counties.
In 1998, Little Rock health plans and providers were optimistic that partnerships
with national firms would bolster their ability to challenge the powerful positions
of the market’s dominant health plan and provider system, Arkansas Blue Cross
Blue Shield (ABCBS) and Baptist Health System. Two years later, optimism has
faded as many of these would-be competitors face mounting financial and operational
problems, eroding their competitive potential. The departure of various health
insurers since 1998 has further constrained competition. As health care costs
increase and premiums rise, many observers fear that health insurance coverage
will become increasingly prohibitive for some consumers, leading to more uninsurance
in the state, where nearly one in seven persons currently goes without coverage.
Other important developments in Little Rock since 1998 include:
- Expansion of specialty services and capacity threatens to erode local hospitals’
revenue base.
- Premiums have escalated, as cost controls remain elusive.
- Financial problems have plagued the area’s predominant safety net provider.
ABCBS and Baptist Remain Powerful as Competitors Flail
 ittle Rock’s health care market continues
to be dominated by ABCBS and Baptist
Health System, and their market positions
are bolstered by a close alliance. Since 1994,
ABCBS and Baptist have had a 50/50 joint
venture in the area’s largest health maintenance
organization (HMO), Health
Advantage HMO, and Baptist provides the
majority of services to members enrolled
in ABCBS’s HMO and PPO products.
The alliance reflects a statewide strategy
on the part of ABCBS to contract exclusively
with regionally dominant hospitals.
Some observers believe that these alliances
offer consumers a high-quality network at
a competitive price. Others say the alliances
inhibit competition and may eventually
lead to higher costs for consumers.
In Little Rock, the ABCBS-Baptist
affiliation has remained a powerful force
in the market, while financial and operational
problems have plagued other plans
and hospitals.
Plan Competition. ABCBS has more than 40 percent of the HMO market share
in Little Rock and close to 60 percent statewide. Much of the plan’s strength,
however, derives from its preferred provider organization (PPO), which has more
than 2.5 times the enrollment of its HMO, or approximately 440,000 enrollees statewide.
ABCBS’s closest HMO competitor
in Little Rock is United Healthcare,
which has a 25 percent share of local
HMO enrollees, but its visibility in the
market appears to be diminishing. Last
year, United combined its Arkansas and
Tennessee plans and moved many operations
to Tennessee, leading some observers
to question whether the plan intends to
remain in the Little Rock market.
Also on questionable footing is Little
Rock’s third-largest HMO, QCA QualChoice
Health Plan, with 19 percent local HMO
market share. Two years ago, this plan,
which is owned by the University of
Arkansas Medical Sciences (UAMS),
Tenet Healthcare Corp., and other equity
partners, was positioning itself to compete
more aggressively with the ABCBS-Baptist
alliance. Now, however, the plan
appears to be financially unstable, and
observers say that it may have been insolvent
at times because of difficulties in meeting
state risk reserve requirements. Whether
QualChoice’s equity partners will provide
additional funding is not known, and
observers suggest that a change for the
plan-perhaps new ownership or, in a
worst-case scenario, dissolution-may be
forthcoming.
Meanwhile, in December 2000,
CIGNA pulled out of the Arkansas HMO
market, affecting approximately 11,000
enrollees (some of whom switched to
CIGNA’s PPO or indemnity products the
plan continues to offer). Although CIGNA
was not a major player in Little Rock when
it exited the market, its departure was significant
in that it decreased the number of
health insurance options available to consumers
and reduced competition.
In all, approximately 40 insurers have
reportedly left the Arkansas market since
1998. Although it is unclear whether all of
these insurers offered health insurance
coverage, most observers agree that health
plan competition has decreased. Besides
CIGNA, other notable health plan exits
during the past two years include American
Investors Life and American Healthcare
Providers, Inc., each of which had close
to 20,000 PPO or HMO enrollees at peak
enrollment. Apart from Blue Cross Blue
Shield of Missouri, which entered the
market with HMO and PPO products,
no new plans have entered the Little Rock
market since 1998. Arkansas’ small size
and relatively rural demographics, along
with the poor health and lower socioeconomic
status of its population, have made
the state a less attractive place for health
plans to enter and operate.
Hospital Competition. Competition also has faltered in Little Rock’s hospital
market, and Baptist has maintained a significant competitive advantage. Although
Baptist’s market share in Little Rock proper is similar to that of its nearest
competitor, St. Vincent’s Health System, Baptist attracts significant additional
volume from referrals from 80 affiliated facilities located throughout the state.
To counter this competitive advantage, St. Vincent’s has invested in NovaSys Health
Network, a statewide provider network created in 1996 that includes 6,000 physicians
and 90 acute care hospitals. Despite its arrangement with NovaSys, St. Vincent’s
has not been as successful as Baptist in attracting referrals from outside the
market.
Moreover, recent financial and
operational problems have eroded the
competitive position of St. Vincent’s.
After providing an infusion of capital,
the Denver-based Catholic Health
Initiatives, which has owned St. Vincent’s
since 1997, curtailed additional support
because of its own financial losses.
Meanwhile, St. Vincent’s has experienced
declining volume in cardiac surgery following
the pullout of a major cardiology group
in 1997 that left to form the Arkansas
Heart Hospital. Additionally, St. Vincent’s
1998 acquisition of another local hospital
has reportedly further strained its
finances. At the same time, St. Vincent’s
has experienced staff reductions and
multiple changes in executive management
over the past two years, and, in
June 2000, it became the first private
Arkansas hospital with a unionized
nursing workforce, following a legal
challenge by the National Labor
Relations Board. ittle Rock’s health care market continues
to be dominated by ABCBS and Baptist
Health System, and their market positions
are bolstered by a close alliance. Since 1994,
ABCBS and Baptist have had a 50/50 joint
venture in the area’s largest health maintenance
organization (HMO), Health
Advantage HMO, and Baptist provides the
majority of services to members enrolled
in ABCBS’s HMO and PPO products.
The alliance reflects a statewide strategy
on the part of ABCBS to contract exclusively
with regionally dominant hospitals.
Some observers believe that these alliances
offer consumers a high-quality network at
a competitive price. Others say the alliances
inhibit competition and may eventually
lead to higher costs for consumers.
In Little Rock, the ABCBS-Baptist
affiliation has remained a powerful force
in the market, while financial and operational
problems have plagued other plans
and hospitals.
Plan Competition. ABCBS has more than 40 percent of the HMO market share
in Little Rock and close to 60 percent statewide. Much of the plan’s strength,
however, derives from its preferred provider organization (PPO), which has more
than 2.5 times the enrollment of its HMO, or approximately 440,000 enrollees statewide.
ABCBS’s closest HMO competitor
in Little Rock is United Healthcare,
which has a 25 percent share of local
HMO enrollees, but its visibility in the
market appears to be diminishing. Last
year, United combined its Arkansas and
Tennessee plans and moved many operations
to Tennessee, leading some observers
to question whether the plan intends to
remain in the Little Rock market.
Also on questionable footing is Little
Rock’s third-largest HMO, QCA QualChoice
Health Plan, with 19 percent local HMO
market share. Two years ago, this plan,
which is owned by the University of
Arkansas Medical Sciences (UAMS),
Tenet Healthcare Corp., and other equity
partners, was positioning itself to compete
more aggressively with the ABCBS-Baptist
alliance. Now, however, the plan
appears to be financially unstable, and
observers say that it may have been insolvent
at times because of difficulties in meeting
state risk reserve requirements. Whether
QualChoice’s equity partners will provide
additional funding is not known, and
observers suggest that a change for the
plan-perhaps new ownership or, in a
worst-case scenario, dissolution-may be
forthcoming.
Meanwhile, in December 2000,
CIGNA pulled out of the Arkansas HMO
market, affecting approximately 11,000
enrollees (some of whom switched to
CIGNA’s PPO or indemnity products the
plan continues to offer). Although CIGNA
was not a major player in Little Rock when
it exited the market, its departure was significant
in that it decreased the number of
health insurance options available to consumers
and reduced competition.
In all, approximately 40 insurers have
reportedly left the Arkansas market since
1998. Although it is unclear whether all of
these insurers offered health insurance
coverage, most observers agree that health
plan competition has decreased. Besides
CIGNA, other notable health plan exits
during the past two years include American
Investors Life and American Healthcare
Providers, Inc., each of which had close
to 20,000 PPO or HMO enrollees at peak
enrollment. Apart from Blue Cross Blue
Shield of Missouri, which entered the
market with HMO and PPO products,
no new plans have entered the Little Rock
market since 1998. Arkansas’ small size
and relatively rural demographics, along
with the poor health and lower socioeconomic
status of its population, have made
the state a less attractive place for health
plans to enter and operate.
Hospital Competition. Competition also has faltered in Little Rock’s hospital
market, and Baptist has maintained a significant competitive advantage. Although
Baptist’s market share in Little Rock proper is similar to that of its nearest
competitor, St. Vincent’s Health System, Baptist attracts significant additional
volume from referrals from 80 affiliated facilities located throughout the state.
To counter this competitive advantage, St. Vincent’s has invested in NovaSys Health
Network, a statewide provider network created in 1996 that includes 6,000 physicians
and 90 acute care hospitals. Despite its arrangement with NovaSys, St. Vincent’s
has not been as successful as Baptist in attracting referrals from outside the
market.
Moreover, recent financial and
operational problems have eroded the
competitive position of St. Vincent’s.
After providing an infusion of capital,
the Denver-based Catholic Health
Initiatives, which has owned St. Vincent’s
since 1997, curtailed additional support
because of its own financial losses.
Meanwhile, St. Vincent’s has experienced
declining volume in cardiac surgery following
the pullout of a major cardiology group
in 1997 that left to form the Arkansas
Heart Hospital. Additionally, St. Vincent’s
1998 acquisition of another local hospital
has reportedly further strained its
finances. At the same time, St. Vincent’s
has experienced staff reductions and
multiple changes in executive management
over the past two years, and, in
June 2000, it became the first private
Arkansas hospital with a unionized
nursing workforce, following a legal
challenge by the National Labor
Relations Board.
Expanded Specialty Care Capacity Threatens Hospital Revenue
 ew service capacity in Little Rock and
outlying communities threatens hospitals
with reduced patient volume in tertiary
care and other lucrative services. Since
1998, open-heart surgery programs have
opened in two competing hospitals in
Searcy, an area 45 minutes northeast of
Little Rock. Open-heart surgery programs
now exist in several other Arkansas
cities, and some communities are
beginning to add neonatal intensive
care capacity.
Observers expressed concern that
the limited volume associated with these
community programs poses potential
quality problems. They also fear that this
service expansion, coupled with the higher
overhead structure of these outlying hospitals,
will drive up overall health care
costs in the state. Yet another concern is
that Little Rock hospitals’ loss of tertiary
service volume may constrain the hospitals’
ability to cross-subsidize important,
yet less profitable, services.
The expansion of physician-owned
ambulatory surgery centers (ASCs) also
poses a threat to revenues of Little Rock
hospitals. Six new ASCs have opened since
1998, nearly tripling the number of such
facilities in the market. A few of the ASCs
are multispecialty centers, but most are
limited to a single specialty (e.g., orthopedics,
gastroenterology or otolaryngology).
Three of the ASCs are joint ownership
arrangements between physicians and
hospitals, but the others are physician-owned
or, in one case, owned by a national
firm. In addition, physicians are adding
ancillary services in their private offices
or through freestanding diagnostic centers.
Some say that this build-up of ambulatory
care capacity is a response by specialists
to maintain income levels by supplementing
their revenue with facility fees.
For the past several years, inpatient
capacity has continued to increase in
Little Rock. The Arkansas Heart Hospital
opened in 1997, and there has been a
steady increase in the facility’s number
of staffed beds since then. Additionally,
both Baptist and St. Vincent’s have opened
new inpatient facilities in North Little
Rock since 1998. While Baptist’s facility
was a replacement, St. Vincent’s was an
addition. Both facilities opened with fewer
beds than originally planned, perhaps indicating
that the market is reaching its
upper limit of inpatient capacity. ew service capacity in Little Rock and
outlying communities threatens hospitals
with reduced patient volume in tertiary
care and other lucrative services. Since
1998, open-heart surgery programs have
opened in two competing hospitals in
Searcy, an area 45 minutes northeast of
Little Rock. Open-heart surgery programs
now exist in several other Arkansas
cities, and some communities are
beginning to add neonatal intensive
care capacity.
Observers expressed concern that
the limited volume associated with these
community programs poses potential
quality problems. They also fear that this
service expansion, coupled with the higher
overhead structure of these outlying hospitals,
will drive up overall health care
costs in the state. Yet another concern is
that Little Rock hospitals’ loss of tertiary
service volume may constrain the hospitals’
ability to cross-subsidize important,
yet less profitable, services.
The expansion of physician-owned
ambulatory surgery centers (ASCs) also
poses a threat to revenues of Little Rock
hospitals. Six new ASCs have opened since
1998, nearly tripling the number of such
facilities in the market. A few of the ASCs
are multispecialty centers, but most are
limited to a single specialty (e.g., orthopedics,
gastroenterology or otolaryngology).
Three of the ASCs are joint ownership
arrangements between physicians and
hospitals, but the others are physician-owned
or, in one case, owned by a national
firm. In addition, physicians are adding
ancillary services in their private offices
or through freestanding diagnostic centers.
Some say that this build-up of ambulatory
care capacity is a response by specialists
to maintain income levels by supplementing
their revenue with facility fees.
For the past several years, inpatient
capacity has continued to increase in
Little Rock. The Arkansas Heart Hospital
opened in 1997, and there has been a
steady increase in the facility’s number
of staffed beds since then. Additionally,
both Baptist and St. Vincent’s have opened
new inpatient facilities in North Little
Rock since 1998. While Baptist’s facility
was a replacement, St. Vincent’s was an
addition. Both facilities opened with fewer
beds than originally planned, perhaps indicating
that the market is reaching its
upper limit of inpatient capacity.
Premiums Rise as Cost Controls Falter
 hatever hopes remained in 1998 that
managed care would help to control
health care costs in Little Rock have
dimmed. For 2001, premium increases of
20 percent or more for commercial products
are commonplace. Plans report that
the premium increases are necessitated in
part by rapid increases in the utilization
of both inpatient and ambulatory care
services in Little Rock-already among
the highest in the country. Since 1998,
for example, plans report that 10 to 20
percent increases in the utilization of
ambulatory care services are not uncommon,
noting that the increases for those
in HMOs are larger than for those in
PPOs. Observers say that plans considering
market entry naively believe they can
reduce utilization, when, in fact, no plan
has been able to do so. Expanded capacity,
the availability of complex procedures
like bone marrow transplants, increased
consumer demand and weak managed
care controls are all said to be contributing
to the higher utilization.
Plans’ ability to control utilization also has been complicated by a 1998 Arkansas
law requiring plans that offered only a fully insured, closed-panel HMO to also
offer a point-of-service (POS), PPO or indemnity option to employers. Plans report
that this law has steered enrollment away from traditional gatekeeper HMO products
toward more loosely managed POs and PPO products.
Contributing further to the market’s
escalating premiums are pressures placed
on plans by physicians to maintain high
payment levels. Plans in Little Rock, although
sometimes failing to pay promptly, have
been generous in their payments to physicians.
Within Little Rock’s predominantly
discounted fee-for-service context, physician
payment rates go up to 150 percent
or more of the Medicare fee schedule.
Some observers believe that high physician
payment rates are necessary to help
physicians subsidize care because of the
relatively low reimbursement received for
the state’s Medicare beneficiaries.
Mirroring the experience in the commercial
sector, managed care’s influence
on public sector programs in Little Rock
has been limited. Arkansas’ Medicaid
program relies on a primary care case-management
model, and state officials
say that there are no plans to move to
a risk-based model. There has been an
attempt to introduce managed care for
the Medicare population, but only 4 percent
of beneficiaries statewide have
enrolled. Observers cite Medicare beneficiaries’
preference for Medigap coverage
and negative media coverage of HMOs
as deterrents to enrollment.
Meanwhile, during the past two years,
premiums for Medicare+Choice have risen
124 percent, and this has been without
including prescription drug coverage in
its benefit package. Following United
Healthcare and CIGNA’s departure from
the Medicare+Choice market in 2000,
only ABCBS’s Health Advantage HMO
participates, leading some to question if
the plan will continue to participate. hatever hopes remained in 1998 that
managed care would help to control
health care costs in Little Rock have
dimmed. For 2001, premium increases of
20 percent or more for commercial products
are commonplace. Plans report that
the premium increases are necessitated in
part by rapid increases in the utilization
of both inpatient and ambulatory care
services in Little Rock-already among
the highest in the country. Since 1998,
for example, plans report that 10 to 20
percent increases in the utilization of
ambulatory care services are not uncommon,
noting that the increases for those
in HMOs are larger than for those in
PPOs. Observers say that plans considering
market entry naively believe they can
reduce utilization, when, in fact, no plan
has been able to do so. Expanded capacity,
the availability of complex procedures
like bone marrow transplants, increased
consumer demand and weak managed
care controls are all said to be contributing
to the higher utilization.
Plans’ ability to control utilization also has been complicated by a 1998 Arkansas
law requiring plans that offered only a fully insured, closed-panel HMO to also
offer a point-of-service (POS), PPO or indemnity option to employers. Plans report
that this law has steered enrollment away from traditional gatekeeper HMO products
toward more loosely managed POs and PPO products.
Contributing further to the market’s
escalating premiums are pressures placed
on plans by physicians to maintain high
payment levels. Plans in Little Rock, although
sometimes failing to pay promptly, have
been generous in their payments to physicians.
Within Little Rock’s predominantly
discounted fee-for-service context, physician
payment rates go up to 150 percent
or more of the Medicare fee schedule.
Some observers believe that high physician
payment rates are necessary to help
physicians subsidize care because of the
relatively low reimbursement received for
the state’s Medicare beneficiaries.
Mirroring the experience in the commercial
sector, managed care’s influence
on public sector programs in Little Rock
has been limited. Arkansas’ Medicaid
program relies on a primary care case-management
model, and state officials
say that there are no plans to move to
a risk-based model. There has been an
attempt to introduce managed care for
the Medicare population, but only 4 percent
of beneficiaries statewide have
enrolled. Observers cite Medicare beneficiaries’
preference for Medigap coverage
and negative media coverage of HMOs
as deterrents to enrollment.
Meanwhile, during the past two years,
premiums for Medicare+Choice have risen
124 percent, and this has been without
including prescription drug coverage in
its benefit package. Following United
Healthcare and CIGNA’s departure from
the Medicare+Choice market in 2000,
only ABCBS’s Health Advantage HMO
participates, leading some to question if
the plan will continue to participate.
Employers Shift Costs
 hile they have expressed disappointment
with managed care’s inability to
control costs, employers have not responded
aggressively to rising premiums. Many
large employers have reconfigured their
health benefits by increasing deductibles
and copayments, rather than passing
premium increases along to employees
through increased contributions. With
this strategy, they have essentially shifted
a larger share of the increased costs to
employees who use health services.
A few small employers have responded
to rising premiums by converting their
employees from group to individual coverage
in what observers describe as a form
of defined contribution. Under these
arrangements, the employer provides the
employee with a fixed contribution to help
cover the cost of coverage. The employee
is responsible for all costs beyond the
employer’s fixed contribution and can
choose from among a range of individual
coverage options offered through the
employer that have varying premiums,
deductibles and copayments. Observers
believe several possible future developments
may prompt more employers to
move to some form of defined contribution,
including declining affordability of
health insurance, passage of state mandates
for minimum benefit packages or passage
of federal legislation that increases the
risk of employer liability. hile they have expressed disappointment
with managed care’s inability to
control costs, employers have not responded
aggressively to rising premiums. Many
large employers have reconfigured their
health benefits by increasing deductibles
and copayments, rather than passing
premium increases along to employees
through increased contributions. With
this strategy, they have essentially shifted
a larger share of the increased costs to
employees who use health services.
A few small employers have responded
to rising premiums by converting their
employees from group to individual coverage
in what observers describe as a form
of defined contribution. Under these
arrangements, the employer provides the
employee with a fixed contribution to help
cover the cost of coverage. The employee
is responsible for all costs beyond the
employer’s fixed contribution and can
choose from among a range of individual
coverage options offered through the
employer that have varying premiums,
deductibles and copayments. Observers
believe several possible future developments
may prompt more employers to
move to some form of defined contribution,
including declining affordability of
health insurance, passage of state mandates
for minimum benefit packages or passage
of federal legislation that increases the
risk of employer liability.
Safety Net Struggles
 ike most hospitals in Little Rock, the
market’s leading provider of indigent
care, UAMS, has been hard hit by substantial
cuts in Medicare reimbursement
brought about by the Balanced Budget
Act of 1997. An accounting error that
resulted in a controversial write-off
of $113 million in uncollectable patient
accounts also created difficulty for the
hospital, as did its continued ownership
interest in financially troubled
QualChoice.
In 2000, some financial relief for
UAMS came with a $2 million appropriation
from the state’s General Improvement
Fund for indigent care services, but the
one-time cash infusion covers only a fraction
of the $20 to $25 million losses the
hospital incurred in each of the two previous
years. Some express concern about
UAMS’s continuing financial instability,
because-other than the Arkansas Children’s
Hospital and a few free and church-based
clinics that operate with limited hours-
UAMS is the predominant safety net
provider for adults in Little Rock.
The Arkansas Children’s Hospital,
a key Little Rock safety net provider for
children, has fared better financially than
UAMS, in part because of its specialized
pediatric services. The Arkansas Children’s
Hospital has been successful in securing
numerous managed care contracts, including one with ABCBS, and is the plan’s
only HMO in-network hospital in Little
Rock other than Baptist. State efforts,
such as the State Children’s Health
Insurance Program (SCHIP), have
reduced the number of uninsured children
and helped to maintain UAMS’s
financial health.
Arkansas has relied largely on outside
monies such as SCHIP and, more recently,
tobacco settlement funds to finance initiatives
aimed at reducing the 15 percent
of the population who are uninsured. Since
Arkansas’ SCHIP program, ARKids
1st, began in 1997, the program has
enrolled more than 70,000 previously
uninsured children. Many believe that,
despite the state’s continuing high rate
of uninsurance, almost all children now
have the opportunity to obtain some
form of coverage.
Currently, however, the state and
federal governments are embroiled in a
contentious disagreement over regulations
that require all children eligible for
Medicaid to be enrolled in that program
instead of ARKids 1st. The federal government
maintains that Medicaid-eligible
children are entitled to the comparatively
more expansive Medicaid benefit package
than what they would receive through
ARKids 1st. The state, on the other hand,
argues that its current policy boosts the
number of children with some form of
coverage, because it does not carry with it
the stigma that is often associated with
Medicaid. State officials hope that the
Bush administration signals new leeway
for state preferences and, thus, receptiveness
to the state’s position within the
federal government.
In another initiative aimed at reducing
the number of uninsured, Arkansas
voters approved a ballot initiative during
the November 2000 election directing 30
percent of the state’s average annual
tobacco settlement of $62 million ($1.62
billion over 25 years) to expand Medicaid
eligibility for adults. Under the expansion,
approximately 40,000 additional adults
could become eligible for Medicaid. ike most hospitals in Little Rock, the
market’s leading provider of indigent
care, UAMS, has been hard hit by substantial
cuts in Medicare reimbursement
brought about by the Balanced Budget
Act of 1997. An accounting error that
resulted in a controversial write-off
of $113 million in uncollectable patient
accounts also created difficulty for the
hospital, as did its continued ownership
interest in financially troubled
QualChoice.
In 2000, some financial relief for
UAMS came with a $2 million appropriation
from the state’s General Improvement
Fund for indigent care services, but the
one-time cash infusion covers only a fraction
of the $20 to $25 million losses the
hospital incurred in each of the two previous
years. Some express concern about
UAMS’s continuing financial instability,
because-other than the Arkansas Children’s
Hospital and a few free and church-based
clinics that operate with limited hours-
UAMS is the predominant safety net
provider for adults in Little Rock.
The Arkansas Children’s Hospital,
a key Little Rock safety net provider for
children, has fared better financially than
UAMS, in part because of its specialized
pediatric services. The Arkansas Children’s
Hospital has been successful in securing
numerous managed care contracts, including one with ABCBS, and is the plan’s
only HMO in-network hospital in Little
Rock other than Baptist. State efforts,
such as the State Children’s Health
Insurance Program (SCHIP), have
reduced the number of uninsured children
and helped to maintain UAMS’s
financial health.
Arkansas has relied largely on outside
monies such as SCHIP and, more recently,
tobacco settlement funds to finance initiatives
aimed at reducing the 15 percent
of the population who are uninsured. Since
Arkansas’ SCHIP program, ARKids
1st, began in 1997, the program has
enrolled more than 70,000 previously
uninsured children. Many believe that,
despite the state’s continuing high rate
of uninsurance, almost all children now
have the opportunity to obtain some
form of coverage.
Currently, however, the state and
federal governments are embroiled in a
contentious disagreement over regulations
that require all children eligible for
Medicaid to be enrolled in that program
instead of ARKids 1st. The federal government
maintains that Medicaid-eligible
children are entitled to the comparatively
more expansive Medicaid benefit package
than what they would receive through
ARKids 1st. The state, on the other hand,
argues that its current policy boosts the
number of children with some form of
coverage, because it does not carry with it
the stigma that is often associated with
Medicaid. State officials hope that the
Bush administration signals new leeway
for state preferences and, thus, receptiveness
to the state’s position within the
federal government.
In another initiative aimed at reducing
the number of uninsured, Arkansas
voters approved a ballot initiative during
the November 2000 election directing 30
percent of the state’s average annual
tobacco settlement of $62 million ($1.62
billion over 25 years) to expand Medicaid
eligibility for adults. Under the expansion,
approximately 40,000 additional adults
could become eligible for Medicaid.
Issues to Track
 BCBS and Baptist individually and
together, through their alliance, continue
to dominate the Little Rock health care
market, gaining strength as competition
weakens in both the hospital and health
plan sectors. Meanwhile, hospitals are
faced with a different type of threat as
they increasingly confront hospitals in
outlying communities and local physicians
vying for key lucrative services that
were once the exclusive domain of Little
Rock hospitals. These expansions appear
to encourage increased utilization at a
time of slack cost controls in the market.
Double-digit premium increases have
become pervasive, and employers have
begun to respond by shifting more costs
to employees, particularly those using
health services. As costs continue to rise,
many have voiced concern that uninsurance
rates may begin to increase, placing
further strain on an already fragile safety net.
As the health care system in Little
Rock evolves, the following issues will be
important to track: BCBS and Baptist individually and
together, through their alliance, continue
to dominate the Little Rock health care
market, gaining strength as competition
weakens in both the hospital and health
plan sectors. Meanwhile, hospitals are
faced with a different type of threat as
they increasingly confront hospitals in
outlying communities and local physicians
vying for key lucrative services that
were once the exclusive domain of Little
Rock hospitals. These expansions appear
to encourage increased utilization at a
time of slack cost controls in the market.
Double-digit premium increases have
become pervasive, and employers have
begun to respond by shifting more costs
to employees, particularly those using
health services. As costs continue to rise,
many have voiced concern that uninsurance
rates may begin to increase, placing
further strain on an already fragile safety net.
As the health care system in Little
Rock evolves, the following issues will be
important to track:
-
Will greater competition emerge in
Little Rock’s health plan and hospital
markets? What market-driven or regulatory
actions will need to be taken for
this to occur?
- How will the development of tertiary
care services in outlying communities
and the build-up of ambulatory care
capacity by Little Rock’s physicians
affect hospitals’ service volume and
financial viability? Will any steps be
taken to control the market’s capacity
and service expansions?
- Will defined-contribution approaches
gain an additional foothold in the market?
In what other ways will employers
respond to rising premiums? Will premium
increases contribute to a higher
rate of uninsurance?
- How will access to care for the uninsured
be affected by initiatives like
ARKids 1st and Medicaid expansion?
What impact will these initiatives have
on the safety net?
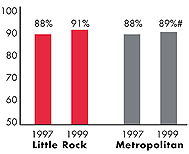
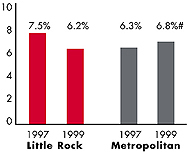
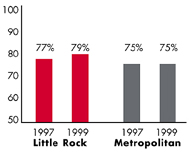
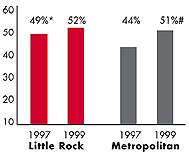
Little Rock’s Experience with the Local Health System, 1997
and 1999
Background and Observations
| Little Rock Demographics |
| Little Rock |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
579,795 |
| Population Change, 1990-19992
|
| 8.4% |
8.6% |
| Median Income3 |
| $28,550 |
$27,843 |
| Persons Living in Poverty3 |
| 12% |
14% |
| Persons Age 65 or Older3 |
| 12% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Little Rock |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 15% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 12% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 82% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $158 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Little Rock |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 5.0 |
2.8 |
| Physicians per 1,000 Population2
|
| 3.1 |
2.3 |
| HMO Penetration, 19973 |
| 25% |
32% |
| HMO Penetration, 19994 |
| 28% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Little Rock Community Report:
Debra A. Draper, Mathematica Policy Research, Inc.
Linda R. Brewster, HSC
Lawrence D. Brown, Columbia University
Lance Heineccius, University of Washington
Carolyn A. Watts, University of Washington
Laurie E. Felland, HSC
Elizabeth Egan, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|