Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Hospitals Profit from Aggressive Negotiations
Miami, Fla.
Community Report No. 10
Summer 2001
Glen P. Mays, Sally Trude, Lawrence P. Casalino, Patricia Lichiello, Ashley C. Short, Andrea Staiti
 n February 2001, a team of
researchers visited Miami, Fla., to
study that community’s health system,
how it is changing and the effects
of those changes on consumers. The
Center for Studying Health System
Change (HSC), as part of the
Community Tracking Study, interviewed
more than 70 leaders in the
health care market. Miami is one of
12 communities tracked by HSC
every two years through site visits and
surveys. Individual community
reports are published for each round
of site visits. The first two site visits to
Miami, in 1996 and 1998, provided
baseline and initial trend information
against which changes are
tracked. The Miami community
encompasses Dade County. n February 2001, a team of
researchers visited Miami, Fla., to
study that community’s health system,
how it is changing and the effects
of those changes on consumers. The
Center for Studying Health System
Change (HSC), as part of the
Community Tracking Study, interviewed
more than 70 leaders in the
health care market. Miami is one of
12 communities tracked by HSC
every two years through site visits and
surveys. Individual community
reports are published for each round
of site visits. The first two site visits to
Miami, in 1996 and 1998, provided
baseline and initial trend information
against which changes are
tracked. The Miami community
encompasses Dade County.
The Miami health care market has become more tumultuous
over the past two years, as key hospitals pressed
health plans for more profitable contracts and, in some
cases, threatened to drop out of plan networks if their
demands were not met. Health maintenance organizations
(HMOs), which dominate the market, experienced financial
losses, leading plans to abandon aggressive price
competition and increase premiums, hitting small businesses
especially hard. Meanwhile, in a market where one
in four persons is uninsured, demand for indigent care
has grown. Though safety net providers have taken steps
to respond, a state health care budget shortfall has created
uncertainty about future funding.
Other important developments in Miami since 1998
include:
- Hospital systems dissolved physician ventures and
abandoned risk contracting because of disappointing
financial performance.
- Health plans introduced less restrictive but costlier
products and retooled provider contracting strategies.
- Affordable insurance options for small businesses eroded,
as the state struggled with insurance reform.
Hospitals Gain Clout
 trengthened by consolidation during the
1990s, Miami’s hospitals have adopted a
tougher negotiating stance with health plans
and have secured payment increases of 15
percent or more over the past year. Two of
the area’s most prominent hospital systems-
Baptist Health System of South Florida and
HCA-The Healthcare Company-publicly
threatened not to renew contracts with
the state’s largest insurer, Blue Cross and
Blue Shield of Florida, unless their
demands for higher payment rates were
met. HCA did the same with two other
large insurers. Most health plans have
yielded to the hospitals’ demands to keep
provider networks intact.
Hospitals reportedly have sought
higher payments from health plans for
several reasons-among them Medicare
payment reductions resulting from the 1997
Balanced Budget Act (BBA), persistently low
payment rates from commercial health plans,
rising uncompensated care expenditures
and losses on risk contracts and business
ventures with physician organizations. In
seeking higher payments, several hospital
systems have benefited from previous
acquisitions and mergers that gave them
considerable influence in geographically
and demographically distinct market niches
within Miami-Dade County. By establishing
these niches, hospital systems such as
Baptist Health System and Tenet Health
System of South Florida have positioned
themselves as highly desirable components
of health plan networks. Hospitals have
gained additional negotiating leverage as
excess capacity has declined in the area due
to continued population growth, hospital
staffing shortages and problems in the state’s
long-term care industry that have reduced
the availability of nursing home beds for
hospitalized patients awaiting discharge.
Miami’s hospital systems also have
used their leverage to abandon unprofitable
risk contracts and to establish more
favorable contracting terms with health
plans. Since 1998, increasing numbers of
hospitals have moved to lucrative per diem
payment arrangements-often with favorable
stop-loss provisions that give a hospital
added financial protection against high-cost
cases. Furthermore, some hospital systems
have convinced plans to discontinue retroactive
denials, a change reinforced by new
state legislation limiting this practice. In
addition, some hospital systems have
successfully prevented plans from excluding
affiliated hospitals from their networks.
As a result of these changes, as well as
steps to strengthen profitable acute care
and specialty service lines, all four of Miami’s
major hospital systems were profitable as of
2001, with both nonprofit Baptist Health
System and county-owned Jackson Memorial
Hospital rebounding from operating losses
in 1999. Some observers indicated that this
success has enabled hospitals to become
more selective in the types of health plans
and contracting arrangements they will
accept. Nevertheless, some health plans
expected that recent improvements in hospital
profitability would ultimately make
contracting negotiations between hospitals
and plans less contentious. trengthened by consolidation during the
1990s, Miami’s hospitals have adopted a
tougher negotiating stance with health plans
and have secured payment increases of 15
percent or more over the past year. Two of
the area’s most prominent hospital systems-
Baptist Health System of South Florida and
HCA-The Healthcare Company-publicly
threatened not to renew contracts with
the state’s largest insurer, Blue Cross and
Blue Shield of Florida, unless their
demands for higher payment rates were
met. HCA did the same with two other
large insurers. Most health plans have
yielded to the hospitals’ demands to keep
provider networks intact.
Hospitals reportedly have sought
higher payments from health plans for
several reasons-among them Medicare
payment reductions resulting from the 1997
Balanced Budget Act (BBA), persistently low
payment rates from commercial health plans,
rising uncompensated care expenditures
and losses on risk contracts and business
ventures with physician organizations. In
seeking higher payments, several hospital
systems have benefited from previous
acquisitions and mergers that gave them
considerable influence in geographically
and demographically distinct market niches
within Miami-Dade County. By establishing
these niches, hospital systems such as
Baptist Health System and Tenet Health
System of South Florida have positioned
themselves as highly desirable components
of health plan networks. Hospitals have
gained additional negotiating leverage as
excess capacity has declined in the area due
to continued population growth, hospital
staffing shortages and problems in the state’s
long-term care industry that have reduced
the availability of nursing home beds for
hospitalized patients awaiting discharge.
Miami’s hospital systems also have
used their leverage to abandon unprofitable
risk contracts and to establish more
favorable contracting terms with health
plans. Since 1998, increasing numbers of
hospitals have moved to lucrative per diem
payment arrangements-often with favorable
stop-loss provisions that give a hospital
added financial protection against high-cost
cases. Furthermore, some hospital systems
have convinced plans to discontinue retroactive
denials, a change reinforced by new
state legislation limiting this practice. In
addition, some hospital systems have
successfully prevented plans from excluding
affiliated hospitals from their networks.
As a result of these changes, as well as
steps to strengthen profitable acute care
and specialty service lines, all four of Miami’s
major hospital systems were profitable as of
2001, with both nonprofit Baptist Health
System and county-owned Jackson Memorial
Hospital rebounding from operating losses
in 1999. Some observers indicated that this
success has enabled hospitals to become
more selective in the types of health plans
and contracting arrangements they will
accept. Nevertheless, some health plans
expected that recent improvements in hospital
profitability would ultimately make
contracting negotiations between hospitals
and plans less contentious.
Back to Top
Few Physician Contracting
Organizations Remain
 ith a few notable exceptions, physician
contracting organizations have failed to
survive in Miami. Numerous national
physician practice management companies
had entered the market, and management
service organizations (MSOs) had formed
to manage physicians’ risk contracts
with health plans. Hospitals had developed
physician-hospital organizations
and employed primary care physicians to
manage risk contracts and protect referrals.
However, most of these ventures
quickly proved financially unsuccessful
and were abandoned.
The demise of physician practice management
companies and hospital-physician
ventures in Miami has soured many physicians
on joining groups, and a steady erosion
of risk contracting has left physicians with
fewer reasons to organize. Most physicians
in the area continue to practice solo or in
small partnerships. A few small single-specialty
physician contracting organizations-
including obstetric/gynecological,
anesthesiology and oncology networks-
have survived and gained some leverage
with health plans, but they are notable
exceptions. These organizations have
secured leverage by controlling large shares
of patient volume at specific hospitals or in
specific geographic areas.
As a result of oversupply and lack of
many contracting organizations, physicians
continue to receive low payment rates. For
privately insured patients in HMOs, physicians
often receive 70 to 80 percent of the
Medicare fee schedule. Although their payment
rates have risen modestly over the
past two years, most Miami physicians have
not secured payment increases comparable
to those won by hospitals.
A few single-specialty physician
organizations have succeeded in creating
ambulatory surgery and diagnostic centers
that compete with hospitals for these
services. But because of hospitals’ opposition
and lingering concerns about the
quality of ambulatory centers, many
health plans have been reluctant to
contract with these centers. ith a few notable exceptions, physician
contracting organizations have failed to
survive in Miami. Numerous national
physician practice management companies
had entered the market, and management
service organizations (MSOs) had formed
to manage physicians’ risk contracts
with health plans. Hospitals had developed
physician-hospital organizations
and employed primary care physicians to
manage risk contracts and protect referrals.
However, most of these ventures
quickly proved financially unsuccessful
and were abandoned.
The demise of physician practice management
companies and hospital-physician
ventures in Miami has soured many physicians
on joining groups, and a steady erosion
of risk contracting has left physicians with
fewer reasons to organize. Most physicians
in the area continue to practice solo or in
small partnerships. A few small single-specialty
physician contracting organizations-
including obstetric/gynecological,
anesthesiology and oncology networks-
have survived and gained some leverage
with health plans, but they are notable
exceptions. These organizations have
secured leverage by controlling large shares
of patient volume at specific hospitals or in
specific geographic areas.
As a result of oversupply and lack of
many contracting organizations, physicians
continue to receive low payment rates. For
privately insured patients in HMOs, physicians
often receive 70 to 80 percent of the
Medicare fee schedule. Although their payment
rates have risen modestly over the
past two years, most Miami physicians have
not secured payment increases comparable
to those won by hospitals.
A few single-specialty physician
organizations have succeeded in creating
ambulatory surgery and diagnostic centers
that compete with hospitals for these
services. But because of hospitals’ opposition
and lingering concerns about the
quality of ambulatory centers, many
health plans have been reluctant to
contract with these centers.
Back to Top
HMO Losses Prompt Changes
 arge financial losses have forced health
plans to abandon aggressive price competition
and seek profitability and growth
through changes in product design. Plans
held premiums low through much of the
1990s, despite rising medical care costs, to
gain a foothold in Miami’s oversaturated
HMO market. As a result, annual HMO
losses mounted, peaking at $183 million
statewide in 1999. Since then, several financially
troubled plans dissolved or were
acquired by other plans, but the market has
remained highly competitive, with at least
16 plans operating in Miami.
Consistent with the insurance underwriting
cycle, most plans have raised
premiums substantially over the past year
to compensate for prior-year losses. Annual
premium increases range from 10 percent
for large groups to well over 20 percent for
groups with fewer than 50 employees. To
minimize premium increases, some plans
have moved to reduce utilization and
costs-including reducing provider networks,
strengthening utilization management,
using hospitalists to manage inpatient care
and increasing consumer cost sharing-
despite the objections of some providers
and consumers.
Other plans have sought to increase
profitability and market share by offering
less restrictive health insurance products
as alternatives to traditional gatekeeper
HMOs that have dominated the market.
UnitedHealthcare became Miami’s largest
and fastest-growing HMO-overtaking
plans such as Blue Cross and Blue Shield of
Florida, Humana Medical Plan and AvMed
Health Plan-after introducing a direct-access
HMO product in late 1998. That
United’s enrollment has continued to grow
over the past year-even though premiums
for direct-access products have become
much higher than those for gatekeeper
HMOs-demonstrates the willingness of
many purchasers and consumers to pay
more for less restrictive products.
Several other Miami plans have recently
introduced direct-access products in
response to United’s success.
The growing popularity of direct-access
HMOs has contributed to the
movement away from risk contracting in
Miami because they do not tie patients
and payments to a specific physician or
medical group. Some primary care physicians
reportedly have opposed the move
away from capitation, arguing that discounted
fee-for-service payments are insufficient
to support the full scope of services
formerly provided under capitation.
Historically, Miami’s HMOs relied
either on full-risk contracting with
provider organizations or on primary care
capitation contracts with individual physicians.
Since 1998, however, most hospitals
have discontinued risk-bearing contracts
and have negotiated more lucrative per
diem payments from health plans. Health
plans have retained some risk contracts
with nonhospital-based provider organizations
(such as MSOs) and most capitated
contracts with primary care physicians,
but, according to several health plans, levels
of service have begun to erode under these
arrangements. Consequently, some of the
market’s largest plans have begun to
move back to fee-for-service payment
arrangements with primary care physicians
and to experiment with limited-risk
arrangements (e.g., contact capitation)
for specialists.
Medicare has remained a competitive
and lucrative business line for Miami’s
HMOs, but the generosity of benefits
offered to Medicare beneficiaries has
begun to erode over the past year. The
BBA constrained payment levels and
introduced stricter accounting rules for
Medicare+Choice, causing HMOs’ financial
margins to decline. Nonetheless,
Medicare+Choice payment rates in
Miami have remained among the highest
in the nation because they are based on
the area’s historically high per-capita
Medicare expenditures.
Consequently, Miami’s seniors continue
to pay no premiums for these plans
and to enjoy a broader choice of plans
and a more comprehensive set of benefits
than their counterparts in other markets.
Over the past year, however, several plans
implemented caps on pharmacy benefits
for the first time, and some plans added
or raised copayments for selected services.
Health plans predicted more severe benefit
reductions and the possibility of plan
withdrawals over the next two years if
Medicare+Choice payment increases continue
to lag behind the rates of growth in
medical and pharmaceutical costs. arge financial losses have forced health
plans to abandon aggressive price competition
and seek profitability and growth
through changes in product design. Plans
held premiums low through much of the
1990s, despite rising medical care costs, to
gain a foothold in Miami’s oversaturated
HMO market. As a result, annual HMO
losses mounted, peaking at $183 million
statewide in 1999. Since then, several financially
troubled plans dissolved or were
acquired by other plans, but the market has
remained highly competitive, with at least
16 plans operating in Miami.
Consistent with the insurance underwriting
cycle, most plans have raised
premiums substantially over the past year
to compensate for prior-year losses. Annual
premium increases range from 10 percent
for large groups to well over 20 percent for
groups with fewer than 50 employees. To
minimize premium increases, some plans
have moved to reduce utilization and
costs-including reducing provider networks,
strengthening utilization management,
using hospitalists to manage inpatient care
and increasing consumer cost sharing-
despite the objections of some providers
and consumers.
Other plans have sought to increase
profitability and market share by offering
less restrictive health insurance products
as alternatives to traditional gatekeeper
HMOs that have dominated the market.
UnitedHealthcare became Miami’s largest
and fastest-growing HMO-overtaking
plans such as Blue Cross and Blue Shield of
Florida, Humana Medical Plan and AvMed
Health Plan-after introducing a direct-access
HMO product in late 1998. That
United’s enrollment has continued to grow
over the past year-even though premiums
for direct-access products have become
much higher than those for gatekeeper
HMOs-demonstrates the willingness of
many purchasers and consumers to pay
more for less restrictive products.
Several other Miami plans have recently
introduced direct-access products in
response to United’s success.
The growing popularity of direct-access
HMOs has contributed to the
movement away from risk contracting in
Miami because they do not tie patients
and payments to a specific physician or
medical group. Some primary care physicians
reportedly have opposed the move
away from capitation, arguing that discounted
fee-for-service payments are insufficient
to support the full scope of services
formerly provided under capitation.
Historically, Miami’s HMOs relied
either on full-risk contracting with
provider organizations or on primary care
capitation contracts with individual physicians.
Since 1998, however, most hospitals
have discontinued risk-bearing contracts
and have negotiated more lucrative per
diem payments from health plans. Health
plans have retained some risk contracts
with nonhospital-based provider organizations
(such as MSOs) and most capitated
contracts with primary care physicians,
but, according to several health plans, levels
of service have begun to erode under these
arrangements. Consequently, some of the
market’s largest plans have begun to
move back to fee-for-service payment
arrangements with primary care physicians
and to experiment with limited-risk
arrangements (e.g., contact capitation)
for specialists.
Medicare has remained a competitive
and lucrative business line for Miami’s
HMOs, but the generosity of benefits
offered to Medicare beneficiaries has
begun to erode over the past year. The
BBA constrained payment levels and
introduced stricter accounting rules for
Medicare+Choice, causing HMOs’ financial
margins to decline. Nonetheless,
Medicare+Choice payment rates in
Miami have remained among the highest
in the nation because they are based on
the area’s historically high per-capita
Medicare expenditures.
Consequently, Miami’s seniors continue
to pay no premiums for these plans
and to enjoy a broader choice of plans
and a more comprehensive set of benefits
than their counterparts in other markets.
Over the past year, however, several plans
implemented caps on pharmacy benefits
for the first time, and some plans added
or raised copayments for selected services.
Health plans predicted more severe benefit
reductions and the possibility of plan
withdrawals over the next two years if
Medicare+Choice payment increases continue
to lag behind the rates of growth in
medical and pharmaceutical costs.
Back to Top
Reforms Fail to Prop Up
Small Group Market
 ffordable insurance options for Miami’s
smallest businesses have dwindled over the
past two years, despite several recent state
reform efforts. In 1996, Florida attempted
to expand insurance options for small
businesses of up to 50 people, including
sole proprietors, through legislation that
required guaranteed issue (plans offering
insurance must sell to any purchaser)
and community rating (premiums reflect
average health care costs in the community
rather than group characteristics
and costs).
These reforms, which were expected
to lower insurance costs by creating an
influx of healthy people to the state’s
small group insurance market, instead
triggered adverse selection by attracting
people with significant health care needs.
Faced with rising costs from small group
policies, health plans responded by raising
small group premiums significantly,
pulling out of the market altogether or
limiting exposure to small groups. Some
plans have begun using complex enrollment
processes and eliminating broker
commissions to avoid groups of fewer
than 10 people.
Another state initiative created insurance
purchasing associations to make small
group insurance more affordable, but they
were dissolved in 2000 after several years of
unsuccessful operations. This effort, launched
in 1994, created insurance purchasing associations,
called Community Health Purchasing
Alliances (CHPAs), in 11 districts throughout
Florida. The CHPAs lost an important
political advocate with the 1998 death of
Gov. Lawton Chiles, who reportedly used
his clout to encourage health plan participation.
Before Chiles’ death, the Miami-Dade
CHPA had as many as 21 health
plan offerings, but by April 2000, only
two plans remained. Other reasons cited
for the CHPAs’ failure included: ffordable insurance options for Miami’s
smallest businesses have dwindled over the
past two years, despite several recent state
reform efforts. In 1996, Florida attempted
to expand insurance options for small
businesses of up to 50 people, including
sole proprietors, through legislation that
required guaranteed issue (plans offering
insurance must sell to any purchaser)
and community rating (premiums reflect
average health care costs in the community
rather than group characteristics
and costs).
These reforms, which were expected
to lower insurance costs by creating an
influx of healthy people to the state’s
small group insurance market, instead
triggered adverse selection by attracting
people with significant health care needs.
Faced with rising costs from small group
policies, health plans responded by raising
small group premiums significantly,
pulling out of the market altogether or
limiting exposure to small groups. Some
plans have begun using complex enrollment
processes and eliminating broker
commissions to avoid groups of fewer
than 10 people.
Another state initiative created insurance
purchasing associations to make small
group insurance more affordable, but they
were dissolved in 2000 after several years of
unsuccessful operations. This effort, launched
in 1994, created insurance purchasing associations,
called Community Health Purchasing
Alliances (CHPAs), in 11 districts throughout
Florida. The CHPAs lost an important
political advocate with the 1998 death of
Gov. Lawton Chiles, who reportedly used
his clout to encourage health plan participation.
Before Chiles’ death, the Miami-Dade
CHPA had as many as 21 health
plan offerings, but by April 2000, only
two plans remained. Other reasons cited
for the CHPAs’ failure included:
- lack of authority to negotiate with health
plans over product offerings;
- inability to pool members under a single
master contract;
- adverse selection stemming from too
many plan choices for employees;
- opposition from insurance brokers; and
- administrative problems, including lax
standards for screening out individuals
representing themselves as businesses.
A new Florida law intended to bolster
the small group insurance market allows
plans to establish premiums based on age
and sex and then adjust these premiums
based on health status and prior utilization
within a rate band of 15 percent. To
address adverse selection problems, the law
establishes an enrollment period for one-person
businesses. In addition, it provides
a structure for private nonprofit purchasing
alliances that would have the authority
to combine lives from multiple small businesses
under a single master policy. The
law’s impact remains to be seen.
Back to Top
Safety Net Responds to
Growing Demand for Care
 ontinued population growth has fueled
the demand for charity care, causing hospitals,
community health centers (CHCs)
and other safety net providers to experience
significant increases in uninsured
caseloads. Miami hospitals have been
particularly hard hit, reporting double-digit
increases in uninsured patients
and uncompensated care costs for 1999.
Miami’s largest charity care provider is
Jackson Memorial Hospital, the only hospital
to receive support from two county-funded
indigent care subsidies. The subsidies-one
funded from general county revenues and
the other through a special state-authorized
sales tax-are administered by the Public
Health Trust of Miami-Dade County, an
independent governing board for county
health services. Other local hospitals have
sought a share of the funding, arguing that
indigent care money should follow uninsured
patients wherever they seek care in
the county, particularly since residents in
some areas do not have easy access to
Jackson Memorial facilities.
The Florida Legislature weighed in on
the controversy in 2000 by passing a law
requiring Miami-Dade County to use
some of its indigent care dollars to operate
a county-wide plan for the uninsured.
Asserting that the law violated the county’s
home rule authority, the Miami-Dade
County Commission refused to implement
it. In February 2001, seven local hospitals
filed a suit against the county seeking to
force compliance with the new law, creating
continued uncertainty about the distribution
of Miami’s indigent care funds.
In an effort to enhance its position as a countywide source of care, Jackson Memorial
Hospital-recently renamed Jackson Health System-has strengthened relationships
with several CHCs and has pursued acquisition of a community hospital serving
southern Dade County, an area where Jackson lacks a strong presence. Jackson also
has begun conversations with several community organizations about creating a
pilot managed care plan for the uninsured in southern Dade County. Other hospitals
argue that Jackson’s actions fall far short of the intent of the state’s indigent
care legislation.
In the midst of this controversy,
Miami’s CHCs have expanded their infrastructure,
services and hours to address the
growing demand for community-based
charity care. CHCs have obtained funding
for these expansions from various sources,
including the Public Health Trust, local governments
and federal grant programs. They
also have developed contracts with Medicaid
HMOs and strengthened efforts to enroll
uninsured patients in Medicaid and the
state’s umbrella program for children’s health
insurance, Florida KidCare. Several community
advocacy organizations have augmented
CHC efforts by launching intensive out-reach
and education campaigns to increase
access to health care among Miami’s large
uninsured and immigrant populations. ontinued population growth has fueled
the demand for charity care, causing hospitals,
community health centers (CHCs)
and other safety net providers to experience
significant increases in uninsured
caseloads. Miami hospitals have been
particularly hard hit, reporting double-digit
increases in uninsured patients
and uncompensated care costs for 1999.
Miami’s largest charity care provider is
Jackson Memorial Hospital, the only hospital
to receive support from two county-funded
indigent care subsidies. The subsidies-one
funded from general county revenues and
the other through a special state-authorized
sales tax-are administered by the Public
Health Trust of Miami-Dade County, an
independent governing board for county
health services. Other local hospitals have
sought a share of the funding, arguing that
indigent care money should follow uninsured
patients wherever they seek care in
the county, particularly since residents in
some areas do not have easy access to
Jackson Memorial facilities.
The Florida Legislature weighed in on
the controversy in 2000 by passing a law
requiring Miami-Dade County to use
some of its indigent care dollars to operate
a county-wide plan for the uninsured.
Asserting that the law violated the county’s
home rule authority, the Miami-Dade
County Commission refused to implement
it. In February 2001, seven local hospitals
filed a suit against the county seeking to
force compliance with the new law, creating
continued uncertainty about the distribution
of Miami’s indigent care funds.
In an effort to enhance its position as a countywide source of care, Jackson Memorial
Hospital-recently renamed Jackson Health System-has strengthened relationships
with several CHCs and has pursued acquisition of a community hospital serving
southern Dade County, an area where Jackson lacks a strong presence. Jackson also
has begun conversations with several community organizations about creating a
pilot managed care plan for the uninsured in southern Dade County. Other hospitals
argue that Jackson’s actions fall far short of the intent of the state’s indigent
care legislation.
In the midst of this controversy,
Miami’s CHCs have expanded their infrastructure,
services and hours to address the
growing demand for community-based
charity care. CHCs have obtained funding
for these expansions from various sources,
including the Public Health Trust, local governments
and federal grant programs. They
also have developed contracts with Medicaid
HMOs and strengthened efforts to enroll
uninsured patients in Medicaid and the
state’s umbrella program for children’s health
insurance, Florida KidCare. Several community
advocacy organizations have augmented
CHC efforts by launching intensive out-reach
and education campaigns to increase
access to health care among Miami’s large
uninsured and immigrant populations.
Back to Top
KidCare’s Growing Pains
 ecent state initiatives to expand public
insurance coverage have helped Miami’s
safety net providers. But the rapid growth
in state health care expenditures has
raised questions about the sustainability
of these efforts. Over the past two years,
Florida has significantly expanded eligibility
for Florida KidCare-an umbrella
program supported through joint federal
and state funding for Medicaid and the
State Children’s Health Insurance Program
(SCHIP), as well as through separate state
appropriations. These eligibility expansions,
combined with a recent outreach campaign,
have netted KidCare nearly 74,000 additional
children in Miami since the beginning of
1999, more than double the 35,000 children
originally expected. The massive
influx of new enrollees, plus rising pharmaceutical
costs, has greatly expanded
Florida’s health care budget.
Mounting state budget pressures have stimulated efforts to control health care
spending. To reduce state expenditures that do not draw down federal matching
funds, the Florida Legislature placed a $13.5 million annual limit on state funding
in 2000 for Florida KidCare enrollees who are ineligible for coverage under federal
Medicaid and SCHIP regulations, including non-citizen children, children of state
employees and 19-year-olds. Florida covers these groups with state appropriations-through
an initiative that predates SCHIP and KidCare-but because of the state funding
limit, enrollment in KidCare was capped for these groups after July 1, 2000. A
waiting list of approximately 6,000 enrollees had formed as of February 2001-with
residents of Miami-Dade and two other south Florida counties reportedly comprising
about 75 percent of those waiting.
While Florida has constrained spending
on individuals ineligible for Medicaid
or SCHIP coverage, state Medicaid expenditures
have continued to grow, resulting
in a Medicaid budget shortfall expected to
total $1 billion by mid-2001, according to
some estimates. This shortfall has generated
a variety of proposals to reduce Medicaid
spending, including payment cuts to
providers and health plans and efforts
to increase Medicaid enrollment in HMOs.
In view of Florida’s mounting budget problems,
some observers feared state efforts to
expand public insurance coverage in
Miami have begun to reach their limits. ecent state initiatives to expand public
insurance coverage have helped Miami’s
safety net providers. But the rapid growth
in state health care expenditures has
raised questions about the sustainability
of these efforts. Over the past two years,
Florida has significantly expanded eligibility
for Florida KidCare-an umbrella
program supported through joint federal
and state funding for Medicaid and the
State Children’s Health Insurance Program
(SCHIP), as well as through separate state
appropriations. These eligibility expansions,
combined with a recent outreach campaign,
have netted KidCare nearly 74,000 additional
children in Miami since the beginning of
1999, more than double the 35,000 children
originally expected. The massive
influx of new enrollees, plus rising pharmaceutical
costs, has greatly expanded
Florida’s health care budget.
Mounting state budget pressures have stimulated efforts to control health care
spending. To reduce state expenditures that do not draw down federal matching
funds, the Florida Legislature placed a $13.5 million annual limit on state funding
in 2000 for Florida KidCare enrollees who are ineligible for coverage under federal
Medicaid and SCHIP regulations, including non-citizen children, children of state
employees and 19-year-olds. Florida covers these groups with state appropriations-through
an initiative that predates SCHIP and KidCare-but because of the state funding
limit, enrollment in KidCare was capped for these groups after July 1, 2000. A
waiting list of approximately 6,000 enrollees had formed as of February 2001-with
residents of Miami-Dade and two other south Florida counties reportedly comprising
about 75 percent of those waiting.
While Florida has constrained spending
on individuals ineligible for Medicaid
or SCHIP coverage, state Medicaid expenditures
have continued to grow, resulting
in a Medicaid budget shortfall expected to
total $1 billion by mid-2001, according to
some estimates. This shortfall has generated
a variety of proposals to reduce Medicaid
spending, including payment cuts to
providers and health plans and efforts
to increase Medicaid enrollment in HMOs.
In view of Florida’s mounting budget problems,
some observers feared state efforts to
expand public insurance coverage in
Miami have begun to reach their limits.
Back to Top
Issues to Track
 rowing hospital negotiating power in
Miami, combined with health plans’ decisions
to offer less restrictive and more
expensive products, has heightened concerns
about the affordability of health
insurance for Miami residents. Florida’s
past efforts to make insurance more
affordable for small businesses have failed,
and the state’s recent public insurance
expansions appear vulnerable to budget
difficulties. With one in four people already
uninsured, any erosion in employer-based
or public coverage could stretch the safety
net beyond its limits. Together, these developments
raise new questions about how
health care delivery and health insurance
coverage may change in Miami: rowing hospital negotiating power in
Miami, combined with health plans’ decisions
to offer less restrictive and more
expensive products, has heightened concerns
about the affordability of health
insurance for Miami residents. Florida’s
past efforts to make insurance more
affordable for small businesses have failed,
and the state’s recent public insurance
expansions appear vulnerable to budget
difficulties. With one in four people already
uninsured, any erosion in employer-based
or public coverage could stretch the safety
net beyond its limits. Together, these developments
raise new questions about how
health care delivery and health insurance
coverage may change in Miami:
- Will consumers and employers continue
to move to direct-access products, despite
rising health care costs and premiums?
- How will rising health insurance premiums
affect private health insurance
coverage, especially for small businesses?
- How will Florida’s new small group insurance
reforms affect small employers’
access to affordable coverage?
- How will hospitals, policy makers and the
Public Health Trust resolve the longstanding
controversy over public funding for
indigent care, and what impact will their
decisions have on access to care for the
uninsured?
- How will state budget pressures affect
benefits and coverage under Florida’s
Medicaid and SCHIP expansion programs,
and how will safety net providers
be affected?
Back to Top
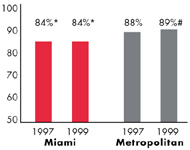
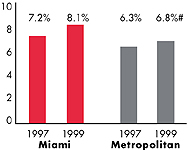
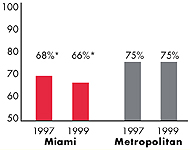
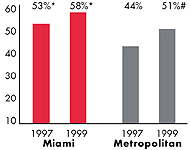
Miami’s Experience with the Local Health System, 1997 and 1999
Back to Top
Background and Observations
| Miami Demographics |
| Miami County |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
2,175,634 |
| Population Change, 1990-19992
|
| 12% |
8.6% |
| Median Income3 |
| $19,672 |
$27,843 |
| Persons Living in Poverty3 |
| 25% |
14% |
| Persons Age 65 or Older3 |
| 15% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Miami |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 23% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 17% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 77% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $161 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Miami |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 3.6 |
2.8 |
| Physicians per 1,000 Population2
|
| 2.7 |
2.3 |
| HMO Penetration, 19973 |
| 64% |
32% |
| HMO Penetration, 19994 |
| 52% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |
Back to Top

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Miami Community Report:
Glen P. Mays, Mathematica Policy Research, Inc.
Sally Trude, HSC
Lawrence P. Casalino, University of Chicago
Patricia Lichiello, University of Washington
Ashley C. Short, HSC
Andrea Benoit, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|