Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Financial Woes and Contract Disputes Disrupt Market
Boston, Mass.
Community Report No. 11
Summer 2001
Kelly Devers, Jon B. Christianson, Laurie E. Felland, Suzanne Felt-Lisk, Liza Rudell, Linda R. Brewster, Ha T. Tu
 n February 2001, a team of
researchers visited Boston, Mass., to
study that community’s health care
system, how it is changing and the
effects of those changes on consumers.
The Center for Studying Health
System Change (HSC), as part of the
Community Tracking Study, interviewed
more than 95 leaders in the
health care market. Boston is one of
the 12 communities tracked by HSC
every two years through site visits and
surveys. Individual community reports
are published for each round of site
visits. The first two site visits to
Boston, in 1996 and 1998, provided
baseline and initial trend information
against which changes are
tracked. The Boston market includes
the city of Boston and Bristol, Essex,
Middlesex, Norfolk, Plymouth and
Suffolk counties. n February 2001, a team of
researchers visited Boston, Mass., to
study that community’s health care
system, how it is changing and the
effects of those changes on consumers.
The Center for Studying Health
System Change (HSC), as part of the
Community Tracking Study, interviewed
more than 95 leaders in the
health care market. Boston is one of
the 12 communities tracked by HSC
every two years through site visits and
surveys. Individual community reports
are published for each round of site
visits. The first two site visits to
Boston, in 1996 and 1998, provided
baseline and initial trend information
against which changes are
tracked. The Boston market includes
the city of Boston and Bristol, Essex,
Middlesex, Norfolk, Plymouth and
Suffolk counties.
After a period of relative stability, Boston’s health care
market was disrupted over the past two years by financial
difficulties in the plan and hospital sectors and
contentious contract disputes between the largest care
system and local plans. Policy makers rapidly enacted
legislation to stabilize the market and took action to
ensure consumers’ access to health care.
In the interest of helping local, not-for-profit plans
regain their financial footing, employers accepted double-digit
premium increases. Consumers continued to enjoy
relatively rich benefits but faced higher copayments for
prescription drugs and outpatient services. Other
important developments include:
- Health maintenance organizations (HMOs) continued
to dominate the plan market but were beginning
to change considerably as plans and providers shed
risk contracts and explored new products and payment
arrangements.
- A state ballot initiative for universal health care
coverage was narrowly defeated, but it prompted the
Massachusetts Legislature to pass a long-debated
patients’ bill of rights.
- Safety net providers, with strong state support and
sound management, remained relatively stable.
Plans and Community Hospitals Experience Financial Distress
 t the time of HSC’s 1998 site visit, Boston’s health care
market had reached relative equilibrium after multiple mergers and acquisitions
left the market consolidated largely around three locally operated, not-for-profit
health plans and two large academic medical center (AMC)-based provider systems.
Since then, a series of events has upset the fragile balance among these organizations,
threatening disruptions for consumers and prompting policy makers to intervene.
Leading Plans Falter. Two local, not-for-profit health plans with national
reputations as pioneering, high-quality HMOs-Harvard Pilgrim Health Care (HPHC)
and Tufts Health Plan-experienced serious financial problems. Both HPHC and Tufts
have long been a source of local pride. Their local roots and not-for- profit
status have been important features in the eyes of policy makers and local providers,
who have been wary of national, for-profit firms. The financial difficulties of
these plans created uncertainty for the roughly 1.8 million enrollees the plans
covered in Massachusetts at their peak and raised questions about the continuing
viability of locally owned, not-for-profit health plans. HPHC and Tufts lost their
position as market leaders as consumers switched to more stable health insurance
options.
HPHC’s severe financial difficulties
were exposed in late 1999, when the plan
unexpectedly posted a $226 million loss.
The state intervened swiftly, placing the
plan into receivership and thereby preventing
disruptions of care for consumers and
a much-feared acquisition by a national,
for-profit insurer. After restructuring the
plan’s debt and allowing certain accounting
changes, the state placed the plan under
administrative supervision and will continue
to monitor its financial status until 2002.
One of HPHC’s downfalls was its
attempt to expand regionally. Since 1999,
HPHC has withdrawn from neighboring
states and reduced its staff substantially. It
also has moved to bring costs under control
by adopting a three-tier pharmacy
benefit, capping Medicare prescription
drug coverage and investing in information
technology to improve its relationships
with providers and consumers. HPHC’s
turnaround efforts appear to be working,
and the plan posted a small operating profit
in the first quarter of 2001. HPHC lost
approximately 700,000 members as a result
of its withdrawal from other New England
states and declines in local membership,
however, and some observers question
whether growing costs will outpace the
plan’s declining revenue.
Tufts’ financial problems also were
associated with failed regional expansion
efforts. The plan posted a $42 million loss
in 1999 and responded, like HPHC, by
reducing staff and withdrawing from three
neighboring states. Although Tufts lost an
estimated 122,000 members and saw its
reserves decline significantly, the plan is
now considered relatively stable.
The financial woes of HPHC and Tufts
highlighted the limited authority policy makers
had to protect consumers from potentially
large-scale disruptions to care. In late
1999, the Massachusetts Legislature enacted
the HMO Insolvency Act, giving the state
Department of Insurance authority to take
over failing plans to ensure that enrollees
continue to receive health care services.
Community Hospitals Struggle. After struggling for more than a decade,
the financial health of Boston’s community hospitals also has deteriorated over
the last two years, leading two hospitals to close and threatening service reductions
and closures elsewhere. Community hospitals’ financial woes stem from a variety
of problems. First, as in many markets nationally, hospitals in Boston have faced
declining reimbursement from private and public payers, increasing labor and pharmaceutical
costs and losses from unsuccessful merger and physician integration strategies.
Second, patients’ growing preference for the Boston area’s prestigious AMCs-the
so-called flight to quality-reportedly has drained community hospitals’ patient
base and eroded essential revenue. According to the state, teaching hospitals’
share of total inpatient discharges in the Boston area grew from 34 percent in
1990 to 42 percent in 2000. Third, all hospitals are required by the state to
contribute resources to an uncompensated care pool, but many are not reimbursed
for the charity care they provide.
Hallmark Health, a struggling community hospital system in the northern Boston
suburbs, closed inpatient services at its 210-bed Malden campus in 1998 and announced
that it would close outpatient services there in 2001. Hallmark also announced
that, because of its financial difficulties, it would close Everett Whidden, a
121-bed facility in North Boston, this year. Other struggling community hospitals
included Symmes Hospital, a 111-bed freestanding community hospital also in a
northern Boston suburb, which closed in 1999; Quincy City Hospital, a 282-bed
hospital in a southern suburb, which announced in 1999 that it would close; and
a large Catholic community hospital system- Caritas Christi-which announced plans
to reduce services at three of its hospitals.
These actual and threatened hospital
closures raised new concerns about access
to care and costs in a market historically
noted for its excess hospital capacity. One
concern was that closures in particular
communities would limit access to care for
nearby residents, especially those unable to
travel. Another was that the growing phenomenon
of emergency room diversions
signaled the possibility of emerging inpatient
capacity constraints that would be
exacerbated by closures and service reductions.
Finally, there was concern that
community hospital closures and service
reductions could accelerate the trend
toward providing routine care in relatively
expensive AMCs.
After Malden and Symmes closed, the public outcry led policy makers and leaders
of local hospitals to save other endangered hospitals. Both the city and the state
intervened with financial assistance to save Quincy City Hospital. In addition,
Quincy entered into an affiliation with Boston Medical Center, a key safety net
hospital system, which allowed the community hospital to remain open, though at
reduced capacity. Cambridge Health Alliance, another major safety net hospital
system, stepped up to help maintain services at Everett Whidden and certain essential
outpatient services at Hallmark’s Malden campus, with the expectation that Cambridge’s
higher Medicare, Medicaid and state uncompensated care pool reimbursements would
help finance these services. Finally, state policy makers helped Caritas Christi
keep its hospital services intact by awarding the system approximately half of
the $10 million distressed hospital funds the state disbursed in 2000.
State policy makers have since taken
steps to ensure that there is greater community
say in reorganizing local health
care services by passing a law that requires
providers to notify the state and hold a
public hearing 90 days before closing
essential community services. Although it
is unclear how far the state might push to
prevent closures, the new law provides a
mechanism to demonstrate the potential
impact of a service cutback on the community
and makes the decision-making
process more transparent.
In addition, policy makers are
grappling with long-term solutions to
hospitals’ financial problems. One strategy
would involve increasing Medicaid reimbursement
rates to cover hospital costs
of care. A recent report commissioned by
the Legislature concluded that this would
cost $200 million annually. However,
some observers note that pressure on
Medicaid to address severe financial
problems in the state’s nursing home
industry may take precedence over payment
increases to hospitals. t the time of HSC’s 1998 site visit, Boston’s health care
market had reached relative equilibrium after multiple mergers and acquisitions
left the market consolidated largely around three locally operated, not-for-profit
health plans and two large academic medical center (AMC)-based provider systems.
Since then, a series of events has upset the fragile balance among these organizations,
threatening disruptions for consumers and prompting policy makers to intervene.
Leading Plans Falter. Two local, not-for-profit health plans with national
reputations as pioneering, high-quality HMOs-Harvard Pilgrim Health Care (HPHC)
and Tufts Health Plan-experienced serious financial problems. Both HPHC and Tufts
have long been a source of local pride. Their local roots and not-for- profit
status have been important features in the eyes of policy makers and local providers,
who have been wary of national, for-profit firms. The financial difficulties of
these plans created uncertainty for the roughly 1.8 million enrollees the plans
covered in Massachusetts at their peak and raised questions about the continuing
viability of locally owned, not-for-profit health plans. HPHC and Tufts lost their
position as market leaders as consumers switched to more stable health insurance
options.
HPHC’s severe financial difficulties
were exposed in late 1999, when the plan
unexpectedly posted a $226 million loss.
The state intervened swiftly, placing the
plan into receivership and thereby preventing
disruptions of care for consumers and
a much-feared acquisition by a national,
for-profit insurer. After restructuring the
plan’s debt and allowing certain accounting
changes, the state placed the plan under
administrative supervision and will continue
to monitor its financial status until 2002.
One of HPHC’s downfalls was its
attempt to expand regionally. Since 1999,
HPHC has withdrawn from neighboring
states and reduced its staff substantially. It
also has moved to bring costs under control
by adopting a three-tier pharmacy
benefit, capping Medicare prescription
drug coverage and investing in information
technology to improve its relationships
with providers and consumers. HPHC’s
turnaround efforts appear to be working,
and the plan posted a small operating profit
in the first quarter of 2001. HPHC lost
approximately 700,000 members as a result
of its withdrawal from other New England
states and declines in local membership,
however, and some observers question
whether growing costs will outpace the
plan’s declining revenue.
Tufts’ financial problems also were
associated with failed regional expansion
efforts. The plan posted a $42 million loss
in 1999 and responded, like HPHC, by
reducing staff and withdrawing from three
neighboring states. Although Tufts lost an
estimated 122,000 members and saw its
reserves decline significantly, the plan is
now considered relatively stable.
The financial woes of HPHC and Tufts
highlighted the limited authority policy makers
had to protect consumers from potentially
large-scale disruptions to care. In late
1999, the Massachusetts Legislature enacted
the HMO Insolvency Act, giving the state
Department of Insurance authority to take
over failing plans to ensure that enrollees
continue to receive health care services.
Community Hospitals Struggle. After struggling for more than a decade,
the financial health of Boston’s community hospitals also has deteriorated over
the last two years, leading two hospitals to close and threatening service reductions
and closures elsewhere. Community hospitals’ financial woes stem from a variety
of problems. First, as in many markets nationally, hospitals in Boston have faced
declining reimbursement from private and public payers, increasing labor and pharmaceutical
costs and losses from unsuccessful merger and physician integration strategies.
Second, patients’ growing preference for the Boston area’s prestigious AMCs-the
so-called flight to quality-reportedly has drained community hospitals’ patient
base and eroded essential revenue. According to the state, teaching hospitals’
share of total inpatient discharges in the Boston area grew from 34 percent in
1990 to 42 percent in 2000. Third, all hospitals are required by the state to
contribute resources to an uncompensated care pool, but many are not reimbursed
for the charity care they provide.
Hallmark Health, a struggling community hospital system in the northern Boston
suburbs, closed inpatient services at its 210-bed Malden campus in 1998 and announced
that it would close outpatient services there in 2001. Hallmark also announced
that, because of its financial difficulties, it would close Everett Whidden, a
121-bed facility in North Boston, this year. Other struggling community hospitals
included Symmes Hospital, a 111-bed freestanding community hospital also in a
northern Boston suburb, which closed in 1999; Quincy City Hospital, a 282-bed
hospital in a southern suburb, which announced in 1999 that it would close; and
a large Catholic community hospital system- Caritas Christi-which announced plans
to reduce services at three of its hospitals.
These actual and threatened hospital
closures raised new concerns about access
to care and costs in a market historically
noted for its excess hospital capacity. One
concern was that closures in particular
communities would limit access to care for
nearby residents, especially those unable to
travel. Another was that the growing phenomenon
of emergency room diversions
signaled the possibility of emerging inpatient
capacity constraints that would be
exacerbated by closures and service reductions.
Finally, there was concern that
community hospital closures and service
reductions could accelerate the trend
toward providing routine care in relatively
expensive AMCs.
After Malden and Symmes closed, the public outcry led policy makers and leaders
of local hospitals to save other endangered hospitals. Both the city and the state
intervened with financial assistance to save Quincy City Hospital. In addition,
Quincy entered into an affiliation with Boston Medical Center, a key safety net
hospital system, which allowed the community hospital to remain open, though at
reduced capacity. Cambridge Health Alliance, another major safety net hospital
system, stepped up to help maintain services at Everett Whidden and certain essential
outpatient services at Hallmark’s Malden campus, with the expectation that Cambridge’s
higher Medicare, Medicaid and state uncompensated care pool reimbursements would
help finance these services. Finally, state policy makers helped Caritas Christi
keep its hospital services intact by awarding the system approximately half of
the $10 million distressed hospital funds the state disbursed in 2000.
State policy makers have since taken
steps to ensure that there is greater community
say in reorganizing local health
care services by passing a law that requires
providers to notify the state and hold a
public hearing 90 days before closing
essential community services. Although it
is unclear how far the state might push to
prevent closures, the new law provides a
mechanism to demonstrate the potential
impact of a service cutback on the community
and makes the decision-making
process more transparent.
In addition, policy makers are
grappling with long-term solutions to
hospitals’ financial problems. One strategy
would involve increasing Medicaid reimbursement
rates to cover hospital costs
of care. A recent report commissioned by
the Legislature concluded that this would
cost $200 million annually. However,
some observers note that pressure on
Medicaid to address severe financial
problems in the state’s nursing home
industry may take precedence over payment
increases to hospitals.
Back to Top
AMCs’ Consolidation Strategies
Yield Mixed Results
 evelopments among Boston’s premier
academic medical systems also caused
considerable turmoil in the market. In
the mid-1990s, many Boston AMCs
embarked on ambitious consolidation
strategies to shore up their positions and
withstand the expected growth of managed
care. For one system, consolidation has
caused serious financial strain, while for
another it has helped to tip the balance of
power away from health plans.
Some of the pitfalls of consolidation
for providers are illustrated by the experience
of CareGroup-a system created out
of the merger of two Harvard Medical
School teaching hospitals, Beth Israel and
New England Deaconess, and a federation
of five affiliated community hospitals. After
the now-combined Beth Israel Deaconess
implemented an ambitious consolidation
and integration strategy, it sustained operating
losses of $215 million over the past
two years and lost substantial market share
as dissatisfied physicians fled the system.
Beth Israel Deaconess hopes to improve its
position by bolstering profitable services
such as cardiology and oncology and pursuing
cost-cutting initiatives. However,
some observers fear that Beth Israel
Deaconess’ sharp financial decline could
have far-reaching effects on the CareGroup
system as a whole. In fact, one community
hospital, Deaconess Waltham, recently
announced the possibility of dropping out
of CareGroup-a move that may signal
substantial changes for the system.
In stark contrast, the experience of
Partners HealthCare illustrates the potential
benefits of consolidation for providers,
along with the potential downside for consumers.
Partners was created in 1994 with
the merger of two prestigious hospitals-
Massachusetts General and Brigham and
Women’s-and now also includes four
community hospitals and several affiliates.
Partners integrated services and facilities
slowly and used the strong affiliation of
member hospitals and 4,000 affiliated
physicians to strengthen its position in
managed care contract negotiations. This
strategy explicitly leveraged the strong
brand-name status of the system’s two
flagship hospitals, while building joint
bargaining power.
Over the past year, the success of this
strategy from the providers’ perspective
became clear, as Partners won payment
increases, reportedly as high as 25 to 30 percent,
from all three of the major local plans: evelopments among Boston’s premier
academic medical systems also caused
considerable turmoil in the market. In
the mid-1990s, many Boston AMCs
embarked on ambitious consolidation
strategies to shore up their positions and
withstand the expected growth of managed
care. For one system, consolidation has
caused serious financial strain, while for
another it has helped to tip the balance of
power away from health plans.
Some of the pitfalls of consolidation
for providers are illustrated by the experience
of CareGroup-a system created out
of the merger of two Harvard Medical
School teaching hospitals, Beth Israel and
New England Deaconess, and a federation
of five affiliated community hospitals. After
the now-combined Beth Israel Deaconess
implemented an ambitious consolidation
and integration strategy, it sustained operating
losses of $215 million over the past
two years and lost substantial market share
as dissatisfied physicians fled the system.
Beth Israel Deaconess hopes to improve its
position by bolstering profitable services
such as cardiology and oncology and pursuing
cost-cutting initiatives. However,
some observers fear that Beth Israel
Deaconess’ sharp financial decline could
have far-reaching effects on the CareGroup
system as a whole. In fact, one community
hospital, Deaconess Waltham, recently
announced the possibility of dropping out
of CareGroup-a move that may signal
substantial changes for the system.
In stark contrast, the experience of
Partners HealthCare illustrates the potential
benefits of consolidation for providers,
along with the potential downside for consumers.
Partners was created in 1994 with
the merger of two prestigious hospitals-
Massachusetts General and Brigham and
Women’s-and now also includes four
community hospitals and several affiliates.
Partners integrated services and facilities
slowly and used the strong affiliation of
member hospitals and 4,000 affiliated
physicians to strengthen its position in
managed care contract negotiations. This
strategy explicitly leveraged the strong
brand-name status of the system’s two
flagship hospitals, while building joint
bargaining power.
Over the past year, the success of this
strategy from the providers’ perspective
became clear, as Partners won payment
increases, reportedly as high as 25 to 30 percent,
from all three of the major local plans:
- Partners adopted an aggressive
negotiating strategy with Blue Cross Blue
Shield of Massachusetts. After six months
of talks, Blue Cross Blue Shield, rather
than risk losing its premier provider,
agreed to large reimbursement increases.
- Next, Partners turned to Tufts in late
2000, reportedly demanding close to a
30 percent reimbursement increase over
three years. After three months of unsuccessful
negotiations, Partners announced
it would not renew its contract and
advised its 100,000 patients covered by
Tufts to make other arrangements for
health care, threatening a major blow to
Tufts as its open-enrollment period
neared. Fearing disruptions for consumers,
the state attorney general and an
influential large employer urged the two
sides to resume negotiations. The dispute
was resolved nine days later, with Tufts
making significant concessions to Partners.
- Finally, Partners made its case to HPHC,
seeking a 28 percent payment increase
over four years. Although the state attorney
general weighed in again-this time
out of concern for the effect of rate
increases on the still-struggling health
plan-Partners again succeeded in securing
significant payment increases.
Partners’ success in winning substantial
payment increases from all three of the
major plans reflects a remarkable power
shift away from health plans. The system
contends that years of steep discounts from
health plans and reduced Medicare and
Medicaid revenue left them no choice but
to push back on commercial plan payment
rates. Health plans caution, however, that
increasing provider reimbursement will
accelerate the trend toward higher premiums.
From the consumer perspective,
Partners’ tactics have created instability
by threatening disruptions to care.
Back to Top
HMOs Undergo Extensive Change
 acing new pressures from providers
and employers, health plans are exploring
innovative ways of managing care and controlling
costs. Risk arrangements have fallen
out of favor with providers, and health plans
have begun to experiment with new product
designs that can accommodate changing
market conditions. Quality improvement
initiatives have received added attention, in
part because of urging from local employers.
Boston has one of the highest HMO
penetration rates in the country, with nearly
50 percent of the population enrolled in
HMOs. Boston HMOs have broad and
overlapping provider networks, few restrictions
on services and rely on discounted
fee-for-service payment arrangements
with withholds contingent on providers’
meeting set utilization targets. Typically,
20 to 30 percent of provider organizations’
total annual compensation is at risk.
For various reasons, providers have not
fared well financially under these payment
arrangements, and some providers have
begun to resist them.
Approximately 29,000 Medicare beneficiaries
in Massachusetts had to switch
plans or select new physicians over the past
year because some providers were unwilling
to accept risk contracts for Medicare
products. Providers are also beginning to
push back on risk in commercial plan
products due in part to tensions over
payment levels and referrals, and many
observers believe this practice will become
widespread. Indeed-in what may prove
to be a harbinger of changes to come-
Partners’ recent contract with HPHC
eliminated withholds that were contingent
on providers’ utilization patterns, replacing
them with bonuses if certain quality standards
are met.
Boston’s employers, while accepting
double-digit premium increases, have
begun to demand patient safety initiatives
and care management programs. The state
employees’ purchasing coalition, which represents
82,000 employees and approximately
250,000 people (about two-thirds of whom
live in Boston), is an example. This coalition
adopted the standards of the Leapfrog
Group-a national organization that advocates
purchasing directives that promote
quality improvement-by including financial
penalties in its recent contracts for plans
failing to reach specified targets for reducing
medical errors. Other employers have urged
plans to supplement their own care management
strategies with programs developed
by national disease management companies
to see which approaches work best.
To help manage costs, plans have
adopted new product designs, including
a three-tier pharmacy benefit and higher
copayments for physician office visits.
Some plans also are exploring the possibility
of a three-tier hospital benefit in which
consumers would pay different amounts,
depending on where they received care. acing new pressures from providers
and employers, health plans are exploring
innovative ways of managing care and controlling
costs. Risk arrangements have fallen
out of favor with providers, and health plans
have begun to experiment with new product
designs that can accommodate changing
market conditions. Quality improvement
initiatives have received added attention, in
part because of urging from local employers.
Boston has one of the highest HMO
penetration rates in the country, with nearly
50 percent of the population enrolled in
HMOs. Boston HMOs have broad and
overlapping provider networks, few restrictions
on services and rely on discounted
fee-for-service payment arrangements
with withholds contingent on providers’
meeting set utilization targets. Typically,
20 to 30 percent of provider organizations’
total annual compensation is at risk.
For various reasons, providers have not
fared well financially under these payment
arrangements, and some providers have
begun to resist them.
Approximately 29,000 Medicare beneficiaries
in Massachusetts had to switch
plans or select new physicians over the past
year because some providers were unwilling
to accept risk contracts for Medicare
products. Providers are also beginning to
push back on risk in commercial plan
products due in part to tensions over
payment levels and referrals, and many
observers believe this practice will become
widespread. Indeed-in what may prove
to be a harbinger of changes to come-
Partners’ recent contract with HPHC
eliminated withholds that were contingent
on providers’ utilization patterns, replacing
them with bonuses if certain quality standards
are met.
Boston’s employers, while accepting
double-digit premium increases, have
begun to demand patient safety initiatives
and care management programs. The state
employees’ purchasing coalition, which represents
82,000 employees and approximately
250,000 people (about two-thirds of whom
live in Boston), is an example. This coalition
adopted the standards of the Leapfrog
Group-a national organization that advocates
purchasing directives that promote
quality improvement-by including financial
penalties in its recent contracts for plans
failing to reach specified targets for reducing
medical errors. Other employers have urged
plans to supplement their own care management
strategies with programs developed
by national disease management companies
to see which approaches work best.
To help manage costs, plans have
adopted new product designs, including
a three-tier pharmacy benefit and higher
copayments for physician office visits.
Some plans also are exploring the possibility
of a three-tier hospital benefit in which
consumers would pay different amounts,
depending on where they received care.
Back to Top
Universal Coverage Initiative
Fails but Prompts New Law
 ealth care advocacy organizations in Massachusetts sponsored
a November 2000 state ballot initiative, known as Question 5, to require the Legislature
to enact universal health care coverage for state residents, and to prohibit for-profit
conversions of health care organizations and implement a patients’ bill of rights.
Plans and employers spent $5 million on an advertising campaign in a successful
effort to defeat the measure. The narrow margin of defeat for the initiative-52
to 48 percent-was viewed as an indication of residents’ continued strong support
for universal health care coverage.
In July 2000, with the ballot measure vote looming, the Legislature passed a long-debated
managed care reform law, known as Chapter 141. If voters had approved the November
2000 initiative, this law would have been superseded. Although Chapter 141 establishes
a commission to research options for universal coverage, the main focus of the
law is on patients’ rights. It calls for an external review process and various
other patient protections short of the right to sue health plans. In addition,
it includes provisions regulating plan-provider payment arrangements. Some observers
believe these payment provisions will dampen plans’ and providers’ willingness
to participate in risk arrangements. One of the most controversial provisions
of Chapter 141 is a requirement that plans send letters to enrollees to inform
them, not only of services that are denied coverage, but also of services that
are approved. Plans contend that this requirement is extremely costly and administratively
burdensome. ealth care advocacy organizations in Massachusetts sponsored
a November 2000 state ballot initiative, known as Question 5, to require the Legislature
to enact universal health care coverage for state residents, and to prohibit for-profit
conversions of health care organizations and implement a patients’ bill of rights.
Plans and employers spent $5 million on an advertising campaign in a successful
effort to defeat the measure. The narrow margin of defeat for the initiative-52
to 48 percent-was viewed as an indication of residents’ continued strong support
for universal health care coverage.
In July 2000, with the ballot measure vote looming, the Legislature passed a long-debated
managed care reform law, known as Chapter 141. If voters had approved the November
2000 initiative, this law would have been superseded. Although Chapter 141 establishes
a commission to research options for universal coverage, the main focus of the
law is on patients’ rights. It calls for an external review process and various
other patient protections short of the right to sue health plans. In addition,
it includes provisions regulating plan-provider payment arrangements. Some observers
believe these payment provisions will dampen plans’ and providers’ willingness
to participate in risk arrangements. One of the most controversial provisions
of Chapter 141 is a requirement that plans send letters to enrollees to inform
them, not only of services that are denied coverage, but also of services that
are approved. Plans contend that this requirement is extremely costly and administratively
burdensome.
Back to Top
Safety Net Strengthened
 n contrast to mainstream providers and plans, Boston’s safety
net providers have been financially strong over the past two years, due in part
to continued state support and sound management strategies. Expansions in Medicaid
and the State Children’s Health Insurance Program and a strong economy also helped
to strengthen the safety net, causing the state’s uninsurance rate to drop considerably.
This trend may continue, given strong legislative support for raising the tobacco
tax an additional 50 cents per pack to extend Medicaid coverage further.
The two major safety net hospital
systems-Boston Medical Center and
Cambridge Health Alliance-continue to
receive the majority of the state’s uncompensated
care and Medicaid disproportionate
share hospital funds. In addition, each hospital
system’s Medicaid managed care plan
has grown because of Medicaid expansions
and entry into new markets outside Boston.
Indeed, the financial strength of these hospitals
was evident in their ability to step in
and help bolster the area’s struggling community
hospitals.
Community health centers (CHCs) in
Boston have become more financially stable
over the past two years, thanks to additional
state funding and new organizational and
management strategies. CHCs benefited
from more than $38 million in new state
funding, as well as increased Medicaid payment
rates for dental services. Although
the state’s largest CHC, East Boston
Neighborhood Health Center, declared
bankruptcy in 1999, it is recovering with
the help of federal and state aid and
improved fiscal management. Finally, some
CHCs have merged or formed alliances to
share overhead expenses and have established
relationships with hospital systems
to obtain assistance for capital improvements
such as information systems. n contrast to mainstream providers and plans, Boston’s safety
net providers have been financially strong over the past two years, due in part
to continued state support and sound management strategies. Expansions in Medicaid
and the State Children’s Health Insurance Program and a strong economy also helped
to strengthen the safety net, causing the state’s uninsurance rate to drop considerably.
This trend may continue, given strong legislative support for raising the tobacco
tax an additional 50 cents per pack to extend Medicaid coverage further.
The two major safety net hospital
systems-Boston Medical Center and
Cambridge Health Alliance-continue to
receive the majority of the state’s uncompensated
care and Medicaid disproportionate
share hospital funds. In addition, each hospital
system’s Medicaid managed care plan
has grown because of Medicaid expansions
and entry into new markets outside Boston.
Indeed, the financial strength of these hospitals
was evident in their ability to step in
and help bolster the area’s struggling community
hospitals.
Community health centers (CHCs) in
Boston have become more financially stable
over the past two years, thanks to additional
state funding and new organizational and
management strategies. CHCs benefited
from more than $38 million in new state
funding, as well as increased Medicaid payment
rates for dental services. Although
the state’s largest CHC, East Boston
Neighborhood Health Center, declared
bankruptcy in 1999, it is recovering with
the help of federal and state aid and
improved fiscal management. Finally, some
CHCs have merged or formed alliances to
share overhead expenses and have established
relationships with hospital systems
to obtain assistance for capital improvements
such as information systems.
Back to Top
Issues to Track
 inancial difficulties among Boston’s health
plans and providers and contentious contract
disputes since 1998 have resulted in
higher premiums for employers and higher
out-of-pocket costs and increasing network
instability for consumers. HMOs have begun
to change considerably, and though use of
risk arrangements and tightly managed
products is waning, there is increased interest
in care management and quality improvement
activities that hold promise for the
future. As the Boston market continues to
evolve, several issues warrant tracking: inancial difficulties among Boston’s health
plans and providers and contentious contract
disputes since 1998 have resulted in
higher premiums for employers and higher
out-of-pocket costs and increasing network
instability for consumers. HMOs have begun
to change considerably, and though use of
risk arrangements and tightly managed
products is waning, there is increased interest
in care management and quality improvement
activities that hold promise for the
future. As the Boston market continues to
evolve, several issues warrant tracking:
- Will plans and community hospitals continue
to experience financial instability,
and, if so, what effects will this have on
the makeup of the health system and continuity
of care for consumers?
- Will threats of care disruption from
health plan-provider contract disputes
become a routine phenomenon in the
Boston health care market, and, if so,
what will the impact be on costs and
consumers’ access to care?
- How will employers respond to rising
premiums, and what effect will their
response have on health plan products?
- Will the state be able to maintain its high
levels of care and coverage for low-income
uninsured despite a potentially
slowing economy?
Back to Top
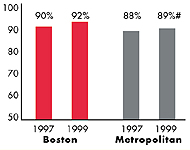
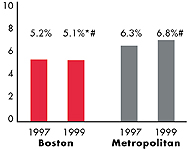
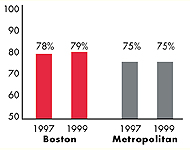
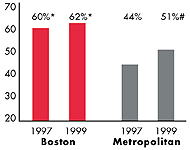
Boston’s Experience with the Local Health System, 1997 and 1999
Back to Top
Background and Observations
| Boston Demographics |
| Boston County |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
4,409,572 |
| Population Change, 1990-19992
|
| 2.8% |
8.6% |
| Median Income3 |
| $31,868 |
$27,843 |
| Persons Living in Poverty3 |
| 10% |
14% |
| Persons Age 65 or Older3 |
| 14% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Boston |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 8.1% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 3.0% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 88% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $198 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Boston |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 2.7 |
2.8 |
| Physicians per 1,000 Population2
|
| 3.3 |
2.3 |
| HMO Penetration, 19973 |
| 46% |
32% |
| HMO Penetration, 19994 |
| 48% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |
Back to Top

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Boston Community Report:
Kelly J. Devers, HSC
Jon B. Christianson, University of Minnesota
Laurie E. Felland, HSC
Sue Felt-Lisk, Mathematica Policy Research, Inc.
Liza S. Rudell, HSC
Linda R. Brewster, HSC
Ha T. Tu, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|