Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Financial Pressures Continue to Plague Hospitals
Northern New Jersey
Community Report No. 12
Summer 2001
Debra A. Draper, Linda R. Brewster, Lawrence D. Brown, Lance Heineccius, Carolyn A. Watts, Elizabeth Eagan, Leslie A. Jackson, Marie C. Reed
 n March 2001, a team of researchers
visited northern New Jersey to study
that community’s health system, how
it is changing and the effects of those
changes on consumers. The Center for
Studying Health System Change
(HSC), as part of the Community
Tracking Study, interviewed more
than 60 leaders in the health care
market. Northern New Jersey is one of
12 communities tracked by HSC
every two years through site visits and
surveys. Individual community reports
are published for each round of site
visits. The first two site visits to
northern New Jersey, in 1997 and
1999, provided baseline and initial
trend information against which
changes are tracked. The northern
New Jersey market encompasses
Essex, Morris, Sussex, Union and
Warren counties. n March 2001, a team of researchers
visited northern New Jersey to study
that community’s health system, how
it is changing and the effects of those
changes on consumers. The Center for
Studying Health System Change
(HSC), as part of the Community
Tracking Study, interviewed more
than 60 leaders in the health care
market. Northern New Jersey is one of
12 communities tracked by HSC
every two years through site visits and
surveys. Individual community reports
are published for each round of site
visits. The first two site visits to
northern New Jersey, in 1997 and
1999, provided baseline and initial
trend information against which
changes are tracked. The northern
New Jersey market encompasses
Essex, Morris, Sussex, Union and
Warren counties.
Since 1999, when hospitals and health plans in northern
New Jersey were struggling with poor financial performance,
many hospitals’ financial problems have worsened.
The state hospital association reports that 60 percent of
New Jersey’s hospitals currently operate in the red. Small
and urban safety net hospitals appear to be the most
severely affected, raising concerns about low-income and
uninsured residents’ continued access to care. In contrast,
most health plans are now financially stable and reporting
profits. Meanwhile, many employers have experienced
double-digit premium increases, and some enrollees
face reduced options as plans become choosier about
their customers and turn down some employers.
Other important developments since 1999 include:
- Health plans shed unprofitable lines of business and
experimented with utilization management strategies
to improve profitability.
- The New Jersey Legislature debated new managed care
laws and added to extensive laws governing health
plans already on the books.
- Public insurance coverage expanded, but key safety net
providers remain on shaky ground.
Urban Hospitals’ Fiscal Health
Remains Critical
 orthern New Jersey has long been noted
for its excess hospital bed capacity and
high utilization of services-both of
which have contributed to higher than
average health care costs. The market’s
inpatient capacity is 36 percent higher
than that of the average metropolitan
market, and its Medicare patients’ hospital
length of stay exceeds the national
average by 50 percent. In the early 1990s,
state policy makers sought to address
these problems by deregulation, replacing
the hospital rate-setting system with a
competitive model to drive down costs.
Since then, hospitals in northern New
Jersey have struggled financially, and significant
efficiencies have not materialized.
In the past two years, hospitals in
the market have continued to be plagued
by financial pressures that stem from
continued low payment rates and rising
operating costs, due in part to a nursing
shortage. In addition, hospitals have seen
their revenues diminish because health
plans have become more aggressive in
their inpatient utilization management
efforts-for example, by significantly
increasing the number of denied days
(days of a hospital stay for which health
plans refuse to pay) and downgraded days
(days reimbursed at a lower rate than usual).
Northern New Jersey’s urban hospitals
are in far worse financial condition
than its suburban-based hospitals, and the
financial gap continues to widen. Urban
hospitals-which constitute the core safety
net for low-income, uninsured individuals-
have been particularly hard hit by
declining patient volume and fewer privately
insured patients. Although many
urban facilities have been financially distressed
for some time, the cumulative
effect of these pressures has heightened
concerns about their viability and implications
for low-income, uninsured patients’
access to care.
Such concerns contributed to a
recent decision to allocate state funds
totaling $9.5 million in 2001 and $5 million
in 2002 to Cathedral Healthcare
System, a Catholic hospital system with
two key safety net facilities in downtown
Newark that were in declining financial
health and threatening to scale back services.
The state also increased its $320
million charity care pool by $36 million
this year-and expects to add $25 million
more in 2002-to assist hospitals serving
the uninsured. Nonetheless, hospital leaders
lament that current state funding for
charity care remains well below the $700
million available before deregulation.
Meanwhile, the finances of northern
New Jersey’s two largest, predominantly
suburban-based hospital systems-St.
Barnabas Health Care System and Atlantic
Health System-are improving. Both systems
were formed in the mid-1990s and,
by 2000, both reported profits, recovering
from previous years’ losses. Their strong
suburban base gives them a more diverse
payer mix, with a higher proportion of
privately insured patients who supply a
steady source of revenue, than their urban
counterparts. Although the suburban
hospital systems have not escaped labor
costs and problems with denied and
downgraded days, they have benefited
from various cost-cutting measures.
In addition, the nine-hospital St.
Barnabas system and four-hospital
Atlantic system have been aggressively
leveraging their size and reputation in
contract negotiations with plans in the
past two years and succeeded in winning
higher payments. Both systems have established
themselves as "must-have" providers
that purchasers insist are included in plan
networks. They also have gained significant
negotiating leverage with plans by moving
to system-wide contracts instead of individually
negotiated contracts for each
affiliated hospital.
Last year, conflict over payment rates
and issues such as utilization management
led to a highly publicized contract dispute
between Atlantic and Aetna U.S. Healthcare.
Both parties made concessions, and new
contract terms were eventually negotiated.
Aetna is reportedly paying significantly
higher rates to Atlantic; Atlantic, in turn,
reportedly signed a multiyear contract,
which helped ensure the stability of
Aetna’s network. orthern New Jersey has long been noted
for its excess hospital bed capacity and
high utilization of services-both of
which have contributed to higher than
average health care costs. The market’s
inpatient capacity is 36 percent higher
than that of the average metropolitan
market, and its Medicare patients’ hospital
length of stay exceeds the national
average by 50 percent. In the early 1990s,
state policy makers sought to address
these problems by deregulation, replacing
the hospital rate-setting system with a
competitive model to drive down costs.
Since then, hospitals in northern New
Jersey have struggled financially, and significant
efficiencies have not materialized.
In the past two years, hospitals in
the market have continued to be plagued
by financial pressures that stem from
continued low payment rates and rising
operating costs, due in part to a nursing
shortage. In addition, hospitals have seen
their revenues diminish because health
plans have become more aggressive in
their inpatient utilization management
efforts-for example, by significantly
increasing the number of denied days
(days of a hospital stay for which health
plans refuse to pay) and downgraded days
(days reimbursed at a lower rate than usual).
Northern New Jersey’s urban hospitals
are in far worse financial condition
than its suburban-based hospitals, and the
financial gap continues to widen. Urban
hospitals-which constitute the core safety
net for low-income, uninsured individuals-
have been particularly hard hit by
declining patient volume and fewer privately
insured patients. Although many
urban facilities have been financially distressed
for some time, the cumulative
effect of these pressures has heightened
concerns about their viability and implications
for low-income, uninsured patients’
access to care.
Such concerns contributed to a
recent decision to allocate state funds
totaling $9.5 million in 2001 and $5 million
in 2002 to Cathedral Healthcare
System, a Catholic hospital system with
two key safety net facilities in downtown
Newark that were in declining financial
health and threatening to scale back services.
The state also increased its $320
million charity care pool by $36 million
this year-and expects to add $25 million
more in 2002-to assist hospitals serving
the uninsured. Nonetheless, hospital leaders
lament that current state funding for
charity care remains well below the $700
million available before deregulation.
Meanwhile, the finances of northern
New Jersey’s two largest, predominantly
suburban-based hospital systems-St.
Barnabas Health Care System and Atlantic
Health System-are improving. Both systems
were formed in the mid-1990s and,
by 2000, both reported profits, recovering
from previous years’ losses. Their strong
suburban base gives them a more diverse
payer mix, with a higher proportion of
privately insured patients who supply a
steady source of revenue, than their urban
counterparts. Although the suburban
hospital systems have not escaped labor
costs and problems with denied and
downgraded days, they have benefited
from various cost-cutting measures.
In addition, the nine-hospital St.
Barnabas system and four-hospital
Atlantic system have been aggressively
leveraging their size and reputation in
contract negotiations with plans in the
past two years and succeeded in winning
higher payments. Both systems have established
themselves as "must-have" providers
that purchasers insist are included in plan
networks. They also have gained significant
negotiating leverage with plans by moving
to system-wide contracts instead of individually
negotiated contracts for each
affiliated hospital.
Last year, conflict over payment rates
and issues such as utilization management
led to a highly publicized contract dispute
between Atlantic and Aetna U.S. Healthcare.
Both parties made concessions, and new
contract terms were eventually negotiated.
Aetna is reportedly paying significantly
higher rates to Atlantic; Atlantic, in turn,
reportedly signed a multiyear contract,
which helped ensure the stability of
Aetna’s network.
Back to Top
Plans Move to Protect Profit,
Exiting Public Programs
 ince 1999, health plans in northern New Jersey have taken
several measures to improve their profitability-including increasing premiums,
shedding unprofitable lines of business and implementing aggressive utilization
management strategies. While such measures have brought greater financial stability
to the plan market, they also have brought rising premiums and fewer options for
Medicare and Medicaid enrollees.
Many health plans have instituted
double-digit premium increases. Employers
in New Jersey’s still-tight labor market have
generally absorbed the premium hikes,
making only modest increases in deductibles
and copayments for employees. Many
plans and employers also have adopted
three-tier pharmacy benefit structures to
combat rapidly rising pharmaceutical costs.
Instead of trying to expand market
share, health plans have been taking a close
look at their portfolios and shedding
unprofitable accounts and lines of business.
As a result, several plans have decided to
abandon the Medicare and Medicaid markets.
Three plans stopped participating in
Medicare+Choice, and others reduced service
areas, citing low payment rates and
onerous program requirements. Currently,
90 percent of northern New Jersey’s 25,000
Medicare+Choice members are enrolled in
either Aetna or Horizon Blue Cross Blue
Shield of New Jersey, but some observers
believe that both plans may be considering
ending their participation in
Medicare+Choice.
Furthermore, Aetna recently
announced it is selling its Medicaid line
of business to AmeriChoice, the second
largest Medicaid plan in northern New
Jersey. As a result, Aetna’s 118,000 Medicaid
enrollees in New Jersey are expected to
move to AmeriChoice. These changes
may be blocked, however, because Aetna
is bound by a consent decree to participate
in Medicare and Medicaid until 2003,
according to the terms of the state’s approval
of Aetna’s recent acquisition of Prudential.
In the past two years, further growth
in health care utilization in northern New
Jersey-already a high-utilization market-
has been reported by health plans. Although
many plans have relaxed preauthorization
and referral requirements in response to
growing market demand for less restrictive
care, they also have implemented
other utilization management strategies
aggressively in an effort to rein in costs.
Many plans have adopted more stringent
utilization management criteria and are
adhering to these standards more strictly.
The result has been a growing number
of denied and downgraded days, which
has angered providers.
Some plans also have increased the
intensity of inpatient utilization management.
Last year, Aetna placed nurses on
site at several hospitals to assist with utilization
management, including discharge
planning, and plans to triple the number
of nurses involved in such utilization
management activities by the end of this
year. Other health plans similarly report
stepped-up activities focusing on discharge
planning. Some hospitals view
these activities as intrusive, but others
reportedly are receptive to having additional
personnel provide assistance,
particularly as hospitals struggle with
a nursing shortage. ince 1999, health plans in northern New Jersey have taken
several measures to improve their profitability-including increasing premiums,
shedding unprofitable lines of business and implementing aggressive utilization
management strategies. While such measures have brought greater financial stability
to the plan market, they also have brought rising premiums and fewer options for
Medicare and Medicaid enrollees.
Many health plans have instituted
double-digit premium increases. Employers
in New Jersey’s still-tight labor market have
generally absorbed the premium hikes,
making only modest increases in deductibles
and copayments for employees. Many
plans and employers also have adopted
three-tier pharmacy benefit structures to
combat rapidly rising pharmaceutical costs.
Instead of trying to expand market
share, health plans have been taking a close
look at their portfolios and shedding
unprofitable accounts and lines of business.
As a result, several plans have decided to
abandon the Medicare and Medicaid markets.
Three plans stopped participating in
Medicare+Choice, and others reduced service
areas, citing low payment rates and
onerous program requirements. Currently,
90 percent of northern New Jersey’s 25,000
Medicare+Choice members are enrolled in
either Aetna or Horizon Blue Cross Blue
Shield of New Jersey, but some observers
believe that both plans may be considering
ending their participation in
Medicare+Choice.
Furthermore, Aetna recently
announced it is selling its Medicaid line
of business to AmeriChoice, the second
largest Medicaid plan in northern New
Jersey. As a result, Aetna’s 118,000 Medicaid
enrollees in New Jersey are expected to
move to AmeriChoice. These changes
may be blocked, however, because Aetna
is bound by a consent decree to participate
in Medicare and Medicaid until 2003,
according to the terms of the state’s approval
of Aetna’s recent acquisition of Prudential.
In the past two years, further growth
in health care utilization in northern New
Jersey-already a high-utilization market-
has been reported by health plans. Although
many plans have relaxed preauthorization
and referral requirements in response to
growing market demand for less restrictive
care, they also have implemented
other utilization management strategies
aggressively in an effort to rein in costs.
Many plans have adopted more stringent
utilization management criteria and are
adhering to these standards more strictly.
The result has been a growing number
of denied and downgraded days, which
has angered providers.
Some plans also have increased the
intensity of inpatient utilization management.
Last year, Aetna placed nurses on
site at several hospitals to assist with utilization
management, including discharge
planning, and plans to triple the number
of nurses involved in such utilization
management activities by the end of this
year. Other health plans similarly report
stepped-up activities focusing on discharge
planning. Some hospitals view
these activities as intrusive, but others
reportedly are receptive to having additional
personnel provide assistance,
particularly as hospitals struggle with
a nursing shortage.
Back to Top
State Increases Health Plan
Regulation
 any states have increased regulation of the managed care industry
in recent years, but, in comparison with the nationally representative sample
of communities that HSC tracks, New Jersey’s regulation is among the most aggressive.
In the past two years, the New Jersey Legislature has enacted new managed care
laws, adding to the already extensive ones on the books.
A broad patients’ rights law with
various consumer protections was passed
in New Jersey in 1997. The law prohibited
gag clauses and mandated access
to specialists and emergency care. It
also expanded state oversight of health
plans’ financial status. In addition, it
established a health plan report card
that documents patient satisfaction and
plan performance on a variety of clinical
measures. Finally, it imposed financial
sanctions on plans that fail to meet
certain performance standards.
In 1998, New Jersey passed regulations,
which became effective in June 2000,
instituting a 10 percent annual penalty for
late payments by plans to providers and
setting a 45-day time limit for providers
to contest claims. To ensure plans’ financial
solvency and avoid problems similar
to those that caused two high-profile plan
failures in 1998, the state recently established
licensure requirements for provider
organizations accepting certain risk
arrangements. In addition, the state has
required that plans contribute $50 million
to a provider bailout fund to help compensate
providers who were left holding
the bag when the two plans folded. Recently,
the New Jersey Legislature passed one of
the strongest managed care laws in the
nation-one that would permit patients
to sue their health maintenance organizations
(HMOs), and the governor signed
the bill into law.
Plans report that they have been reeling
under the onslaught of New Jersey’s
managed care legislation. One plan executive
estimates he spends 20 to 25 percent
of his time addressing regulatory issues-
far more than he spent five years ago.
Another plan noted that changes under
the state’s new prompt-payment requirement
alone have required information
systems’ investments of $1 million. The
fact that New Jersey has put health plans
on a fast track to implement administrative
simplification requirements in the
federal Health Insurance Portability
and Accountability Act (HIPAA) has
created additional cost pressures. One
plan expects that changes necessary to
become HIPAA compliant will be its
single largest expenditure this year.
The pressure on plans to compete in this tough regulatory environment- particularly
with a mounting need for capital-may lead to further consolidation. Northern New
Jersey experienced some plan consolidation over the past few years due to plan
failures, as well as national mergers such as Aetna’s with US Healthcare and,
more recently, with Prudential. Although 13 plans continue to operate in the area,
market share is concentrated among five. Aetna, the leader in the HMO market,
accounts for almost 40 percent of all enrollees.
Horizon Blue Cross Blue Shield
of New Jersey is the only not-for-profit
plan among the top five competitors;
the four others are publicly traded
firms. Competitive pressures may lead
Horizon to renew its efforts, previously
blocked by the state, to convert to for-profit
status. The recent for-profit
conversion of nearby New York City-based
Empire Blue Cross Blue Shield
may lend support to Horizon, if the
plan decides to move in that direction. any states have increased regulation of the managed care industry
in recent years, but, in comparison with the nationally representative sample
of communities that HSC tracks, New Jersey’s regulation is among the most aggressive.
In the past two years, the New Jersey Legislature has enacted new managed care
laws, adding to the already extensive ones on the books.
A broad patients’ rights law with
various consumer protections was passed
in New Jersey in 1997. The law prohibited
gag clauses and mandated access
to specialists and emergency care. It
also expanded state oversight of health
plans’ financial status. In addition, it
established a health plan report card
that documents patient satisfaction and
plan performance on a variety of clinical
measures. Finally, it imposed financial
sanctions on plans that fail to meet
certain performance standards.
In 1998, New Jersey passed regulations,
which became effective in June 2000,
instituting a 10 percent annual penalty for
late payments by plans to providers and
setting a 45-day time limit for providers
to contest claims. To ensure plans’ financial
solvency and avoid problems similar
to those that caused two high-profile plan
failures in 1998, the state recently established
licensure requirements for provider
organizations accepting certain risk
arrangements. In addition, the state has
required that plans contribute $50 million
to a provider bailout fund to help compensate
providers who were left holding
the bag when the two plans folded. Recently,
the New Jersey Legislature passed one of
the strongest managed care laws in the
nation-one that would permit patients
to sue their health maintenance organizations
(HMOs), and the governor signed
the bill into law.
Plans report that they have been reeling
under the onslaught of New Jersey’s
managed care legislation. One plan executive
estimates he spends 20 to 25 percent
of his time addressing regulatory issues-
far more than he spent five years ago.
Another plan noted that changes under
the state’s new prompt-payment requirement
alone have required information
systems’ investments of $1 million. The
fact that New Jersey has put health plans
on a fast track to implement administrative
simplification requirements in the
federal Health Insurance Portability
and Accountability Act (HIPAA) has
created additional cost pressures. One
plan expects that changes necessary to
become HIPAA compliant will be its
single largest expenditure this year.
The pressure on plans to compete in this tough regulatory environment- particularly
with a mounting need for capital-may lead to further consolidation. Northern New
Jersey experienced some plan consolidation over the past few years due to plan
failures, as well as national mergers such as Aetna’s with US Healthcare and,
more recently, with Prudential. Although 13 plans continue to operate in the area,
market share is concentrated among five. Aetna, the leader in the HMO market,
accounts for almost 40 percent of all enrollees.
Horizon Blue Cross Blue Shield
of New Jersey is the only not-for-profit
plan among the top five competitors;
the four others are publicly traded
firms. Competitive pressures may lead
Horizon to renew its efforts, previously
blocked by the state, to convert to for-profit
status. The recent for-profit
conversion of nearby New York City-based
Empire Blue Cross Blue Shield
may lend support to Horizon, if the
plan decides to move in that direction.
Back to Top
Retreat from Managed Care
Strategies
 he current HMO penetration rate in
northern New Jersey, 25 percent, is far
lower than the penetration rate in many
other markets nationally. Despite concerns
about the market’s high costs
and high utilization, HMOs have been
slow to make inroads in northern
New Jersey, largely because many large
employers with highly skilled and often
unionized work forces have favored
less restrictive coverage.
Since 1999, plans in the area have
sought to attract enrollment by introducing
more open-access products that
eliminate gatekeeper requirements. In
addition, some plans are considering
developing hybrid products that allow
direct access to specialists, sometimes
within narrower subnetworks. Many are
also scaling back other restrictive product
features such as preauthorization and
referral requirements.
The recent move by some health
plans to more loosely managed products
has been accompanied by plans’ and
providers’ waning interest in risk-contracting
arrangements, which plans
once advocated as an essential strategy
for engaging providers in controlling
costs. Atlantic invested $20 million in
its physician-hospital contracting entity,
Health Resource Partners, only to have it
close two years later after failing to secure
risk contracts from health plans. St.
Barnabas’ physician-hospital contracting
entity, Physician Partnership, also struggled
without risk contracts and has recently
shifted focus to become the exclusive
network of providers for St. Barnabas
employees under its newly formed self-funded
health insurance plan. Physician
Partnership is the sole option for more
than 22,000 St. Barnabas employees and
their dependents; eventually, the plan
may be marketed to local employer
groups interested in direct contracting.
Several hospitals that had pursued
mergers or affiliations with expectations
of growth in risk contracting have abandoned
these relationships. Chilton
Memorial Hospital and Valley Health
System (located just outside the market
area) decided to go their separate ways
in January 2001 because their more than
three-year affiliation failed to yield any
risk-bearing managed care contracts.
Hudson County’s Bayonne Hospital
recently terminated its affiliation with
Atlantic for similar reasons. Some
observers contend that New Jersey’s
new regulations concerning risk arrangements
have contributed to the decline
of such arrangements. Others note that
providers were slow to develop the
infrastructure to accept risk contracts,
and few risk arrangements ever materialized
in the market. he current HMO penetration rate in
northern New Jersey, 25 percent, is far
lower than the penetration rate in many
other markets nationally. Despite concerns
about the market’s high costs
and high utilization, HMOs have been
slow to make inroads in northern
New Jersey, largely because many large
employers with highly skilled and often
unionized work forces have favored
less restrictive coverage.
Since 1999, plans in the area have
sought to attract enrollment by introducing
more open-access products that
eliminate gatekeeper requirements. In
addition, some plans are considering
developing hybrid products that allow
direct access to specialists, sometimes
within narrower subnetworks. Many are
also scaling back other restrictive product
features such as preauthorization and
referral requirements.
The recent move by some health
plans to more loosely managed products
has been accompanied by plans’ and
providers’ waning interest in risk-contracting
arrangements, which plans
once advocated as an essential strategy
for engaging providers in controlling
costs. Atlantic invested $20 million in
its physician-hospital contracting entity,
Health Resource Partners, only to have it
close two years later after failing to secure
risk contracts from health plans. St.
Barnabas’ physician-hospital contracting
entity, Physician Partnership, also struggled
without risk contracts and has recently
shifted focus to become the exclusive
network of providers for St. Barnabas
employees under its newly formed self-funded
health insurance plan. Physician
Partnership is the sole option for more
than 22,000 St. Barnabas employees and
their dependents; eventually, the plan
may be marketed to local employer
groups interested in direct contracting.
Several hospitals that had pursued
mergers or affiliations with expectations
of growth in risk contracting have abandoned
these relationships. Chilton
Memorial Hospital and Valley Health
System (located just outside the market
area) decided to go their separate ways
in January 2001 because their more than
three-year affiliation failed to yield any
risk-bearing managed care contracts.
Hudson County’s Bayonne Hospital
recently terminated its affiliation with
Atlantic for similar reasons. Some
observers contend that New Jersey’s
new regulations concerning risk arrangements
have contributed to the decline
of such arrangements. Others note that
providers were slow to develop the
infrastructure to accept risk contracts,
and few risk arrangements ever materialized
in the market.
Back to Top
Public Insurance Expands, but
Safety Net Is Shaky
 ew Jersey recently has made significant
strides in expanding public insurance
coverage, following a period of slow
enrollment in the State Children’s Health
Insurance Program (SCHIP). With a
waiver from the Centers for Medicare and
Medicaid Services-formerly the Health
Care Financing Administration-New
Jersey expanded the program to include
adults with incomes up to 200 percent
of the poverty level. The new program,
known as New Jersey FamilyCare, includes
the 70,000 children originally enrolled
in SCHIP. It also will offer coverage to
125,000 low-income, uninsured adults.
The initial demand for New Jersey
FamilyCare has been overwhelming. In
fact, the volume of applications suggests
that the program is fast approaching its
enrollment cap. State officials are grappling
with whether to use waiting lists or
appropriate more funds to expand the
program to include more people. The
state has been financing its share of the
$200 million program with tobacco settlement
monies, employer contributions
and enrollee premiums. A projected state
budget deficit, however, may severely
constrain the state’s ability to find additional
funding.
Meanwhile, the state-owned safety
net provider in Newark, University
Hospital, has become financially stressed
over the past two years. Though improving
now as intensive efforts take hold, this situation
has prompted the state to consider
possible mergers with other downtown
hospitals-either St. Michael’s Medical
Center (part of Cathedral) or Newark
Beth Israel Medical Center (part of St.
Barnabas). Although both potential
merger partners also are longstanding
safety net providers, there is some concern
that a merger would diminish overall
capacity to care for low-income and
uninsured people, particularly in downtown
Newark.
There also is concern that an imminent
plan to establish a new residency
program at the University of Medicine
and Dentistry of New Jersey (UMDNJ)
through the Atlantic Health System will
deplete University Hospital of essential
financial resources and physicians.
UMDNJ is interested in establishing a
suburban affiliation to attract a more
diverse group of residents and compete
more aggressively with academic medical
centers located nearby in New York City
and Philadelphia. For University Hospital,
which has the current local residency
program, such a move could prove challenging.
It might even prompt the state to
move more quickly with its merger plans
for the hospital. ew Jersey recently has made significant
strides in expanding public insurance
coverage, following a period of slow
enrollment in the State Children’s Health
Insurance Program (SCHIP). With a
waiver from the Centers for Medicare and
Medicaid Services-formerly the Health
Care Financing Administration-New
Jersey expanded the program to include
adults with incomes up to 200 percent
of the poverty level. The new program,
known as New Jersey FamilyCare, includes
the 70,000 children originally enrolled
in SCHIP. It also will offer coverage to
125,000 low-income, uninsured adults.
The initial demand for New Jersey
FamilyCare has been overwhelming. In
fact, the volume of applications suggests
that the program is fast approaching its
enrollment cap. State officials are grappling
with whether to use waiting lists or
appropriate more funds to expand the
program to include more people. The
state has been financing its share of the
$200 million program with tobacco settlement
monies, employer contributions
and enrollee premiums. A projected state
budget deficit, however, may severely
constrain the state’s ability to find additional
funding.
Meanwhile, the state-owned safety
net provider in Newark, University
Hospital, has become financially stressed
over the past two years. Though improving
now as intensive efforts take hold, this situation
has prompted the state to consider
possible mergers with other downtown
hospitals-either St. Michael’s Medical
Center (part of Cathedral) or Newark
Beth Israel Medical Center (part of St.
Barnabas). Although both potential
merger partners also are longstanding
safety net providers, there is some concern
that a merger would diminish overall
capacity to care for low-income and
uninsured people, particularly in downtown
Newark.
There also is concern that an imminent
plan to establish a new residency
program at the University of Medicine
and Dentistry of New Jersey (UMDNJ)
through the Atlantic Health System will
deplete University Hospital of essential
financial resources and physicians.
UMDNJ is interested in establishing a
suburban affiliation to attract a more
diverse group of residents and compete
more aggressively with academic medical
centers located nearby in New York City
and Philadelphia. For University Hospital,
which has the current local residency
program, such a move could prove challenging.
It might even prompt the state to
move more quickly with its merger plans
for the hospital.
Back to Top
Issues to Track
 inancial pressures continue to plague
many northern New Jersey hospitals,
leaving some downtown facilities in a
particularly precarious condition and
threatening their capacity to care for low-income
and uninsured people. Health
plans’ financial condition has generally
stabilized, but competitive pressures in an
intense state regulatory environment may
promise change in the plan sector as well.
As plans attempt to restore profitability
and respond to consumer demand for
less restrictive products, it is likely that
employers will face escalating premiums,
making health insurance coverage more
costly. And although New Jersey has
successfully expanded public insurance
options through New Jersey FamilyCare,
state budget constraints may ultimately
limit the reach of this program.
These observations suggest several
important issues to track: inancial pressures continue to plague
many northern New Jersey hospitals,
leaving some downtown facilities in a
particularly precarious condition and
threatening their capacity to care for low-income
and uninsured people. Health
plans’ financial condition has generally
stabilized, but competitive pressures in an
intense state regulatory environment may
promise change in the plan sector as well.
As plans attempt to restore profitability
and respond to consumer demand for
less restrictive products, it is likely that
employers will face escalating premiums,
making health insurance coverage more
costly. And although New Jersey has
successfully expanded public insurance
options through New Jersey FamilyCare,
state budget constraints may ultimately
limit the reach of this program.
These observations suggest several
important issues to track:
- Will New Jersey’s hospitals achieve
financial stability, and, if so, at what
price for the safety net?
- How will health plans continue to deal
with mounting cost pressures? Will
plans continue to withdraw from the
Medicare and Medicaid markets? Will
another wave of plan consolidation
materialize?
- How will employers respond to rising
premiums? Will employers increase cost
sharing for employees? Will greater
pressure emerge to control costs and
utilization, and, if so, how will plans
respond?
- How will the state deal with the overwhelming
demand for coverage under
New Jersey FamilyCare? Will the state’s
projected budget deficit limit this program’s
potential?
Back to Top
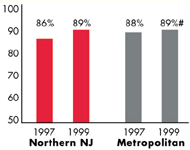
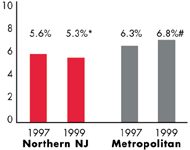
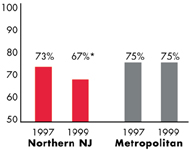
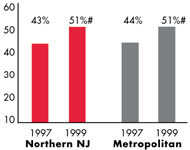
Northern New Jersey’s Experience with the Local Health System, 1997 and 1999
Back to Top
Background and Observations
| Northern New Jersey Demographics |
| Northern New Jersey |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
1,954,671 |
| Population Change, 1990-19992
|
| 2.0% |
8.6% |
| Median Income3 |
| $32,890 |
$27,843 |
| Persons Living in Poverty3 |
| 10% |
14% |
| Persons Age 65 or Older3 |
| 14% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Northern New Jersey |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 12% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 8% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 84% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $198 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Northern New Jersey |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 3.8 |
2.8 |
| Physicians per 1,000 Population2
|
| 2.6 |
2.3 |
| HMO Penetration, 19973 |
| 17% |
32% |
| HMO Penetration, 19994 |
| 25% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |
Back to Top

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Northern New Jersey Community Report:
Debra A. Draper, Mathematica Policy Research, Inc.
Linda R. Brewster, HSC
Lawrence D. Brown, Columbia University
Lance Heineccius, University of Washington
Carolyn A. Watts, University of Washington
Elizabeth Eagan, HSC
Leslie Jackson, HSC
Marie C. Reed, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|