
Limited Information Technology for Patient Care in Physician Offices
Issue Brief No. 89
September 2004
Marie C. Reed, Joy M. Grossman
Evidence of physicians’ use of information technology (IT) to support patient care has been sketchy and anecdotal to date. However, new findings from the Center for Studying Health System Change (HSC) show wide variation in information technology adoption across physician practices, particularly by physician practice size. In 2001, nearly 60 percent of physicians in traditional practice settings—primarily solo or relatively small group practices where the vast majority of Americans receive care—reported that their practice used information technology in no more than one of the five following clinical functions: obtaining treatment guidelines, exchanging clinical data with other physicians, accessing patient notes, generating treatment reminders for the physician’s use and writing prescriptions. Highest levels of IT support for patient care were found in staff- and group-model health maintenance organization (HMO) practices, followed by medical school faculty practices and large group practices. Overall rates of information technology adoption may have increased since 2001, but the variation in IT adoption by practice setting is unlikely to have changed.
- Physicians and Information Technology: A Long Way to Go
- IT Benchmarks
- Practice Size Matters
- Other Factors Play Minor Role
- Policy Options
- Notes
- Data Source
- Supplementary Tables
Physicians and Information Technology: A Long Way to Go
![]() hile the Institute of Medicine (IOM) has identified information
technology as playing a pivotal role in systematically improving the quality
of clinical care and reducing health care costs,1 the health
care industry adopts IT at a relatively slow pace compared with other industries.
Recently, momentum for both public and private initiatives to promote IT adoption
in hospitals and physicians’ offices has been building, and the federal government,
in particular, has stepped up efforts to foster IT adoption.2
hile the Institute of Medicine (IOM) has identified information
technology as playing a pivotal role in systematically improving the quality
of clinical care and reducing health care costs,1 the health
care industry adopts IT at a relatively slow pace compared with other industries.
Recently, momentum for both public and private initiatives to promote IT adoption
in hospitals and physicians’ offices has been building, and the federal government,
in particular, has stepped up efforts to foster IT adoption.2
While the use of IT in physicians’ offices potentially can improve quality and reduce costs, implementation is costly because of up-front investments in capital, training and integrating IT systems with existing administrative and clinical processes. The business case for physician implementation of IT to improve health care quality is still being made, since the benefits of lower costs and improved health are uncertain and generally accrue more directly to health plans, employers and patients than to physicians. As a result, many physician practices may be reluctant to introduce IT practices may be reluctant to introduce IT beyond administrative and management systems that directly affect revenues.
If policy makers want to encourage IT adoption, they need reliable data on physicians’ use of information technology in their practices. By understanding patterns of IT adoption among physicians, policy makers can target efforts at physicians who are likely to be slower in adopting clinical IT systems.
Back to Top
IT Benchmarks
HSC’s 2001 Community Tracking Study (CTS) Physician Survey provides the first nationally representative data on the availability of information technology in physicians’ offices across specialties, practice settings and geographic areas (see Data Source). The 2001 survey information is a useful benchmark, since recent reports indicate considerable physician interest in clinical applications of information technology, but evidence of widespread increases in IT adoption since 2001 is lacking.3 In the survey, physicians were asked whether computers or other forms of information technology were used in their practice to support five clinical functions: obtaining treatment guidelines, exchanging clinical data with other physicians, accessing patient notes, generating treatment reminders for the physician’s use and writing prescriptions.
The use of IT in each of the five areas has been shown to improve the quality of care in at least one of three key quality domains identified by the IOM: effectiveness, timeliness and/or patient safety. While there are other aspects of clinical practice where IT may be useful in improving the quality of care—such as decision support—the five clinical applications represent a broad spectrum of activities relevant to the quality of care provided to patients during office and follow-up visits.
The vast majority of patients were treated in physician practices lacking significant IT support for patient care in 2001. One-quarter of all physicians were in practices with no computer or other form of IT support for any of the five functions, and another quarter had IT available for just one function (see Figure 1). In contrast, about a tenth of physicians were in practices with IT support for four or five functions. Adoption of IT varied considerably by function (see Table 1). Just slightly more than half of physicians reported that their practices used IT to obtain information on treatment guidelines (53%), the highest adoption rate of any of the five functions. Other rates were each less than 50 percent, with electronic prescribing least likely (11%) to be available in physicians’ offices.
Back to Top
Figure 1 |
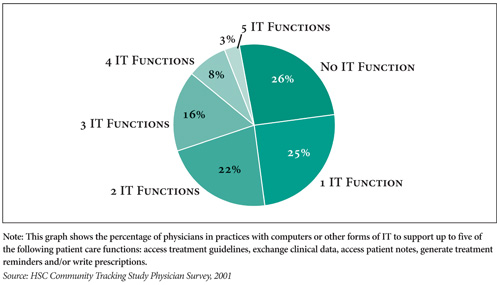 |
Table 1
|
|
Access Treatment Guidelines
|
Exchange Clinical Data
|
Access Patient Notes
|
Generate Treatment Reminders
|
Electronic Prescriptions
|
Distribution of Physicians
|
|
| All |
53%
|
41%
|
37%
|
24%
|
11%
|
100%
|
| Practice Setting | ||||||
| Traditional Practice Setting1 |
50*
|
32*
|
29*
|
23*
|
8*
|
69
|
| Hospital Staff & Other |
55
|
49*
|
41*
|
19*
|
14*
|
16
|
| Large Group (>50 Physicians)2 |
57
|
63
|
58
|
29
|
20
|
3
|
| Medical School |
66*
|
72*
|
66*
|
20*
|
15
|
8
|
| Staff/Group HMO |
76*
|
75*
|
83*
|
59*
|
38*
|
4
|
| Specialty | ||||||
| Primary Care2 |
53
|
36
|
32
|
26
|
13
|
40
|
| Medical or Surgical Specialty |
53
|
44*
|
40*
|
22*
|
11*
|
60
|
| Age | ||||||
| <552 |
55
|
42
|
38
|
23
|
12
|
78
|
| 55+ |
45*
|
34*
|
32*
|
24
|
9*
|
22
|
| Practice Location | ||||||
| Metropolitan Area2 |
53
|
41
|
37
|
23
|
11
|
89
|
| Nonmetropolitan Area |
56
|
33*
|
33
|
25
|
10
|
11
|
| 1 Includes solo and two-physician
practices, groups with 50 or fewer physicians, and physicians in office-based
practices owned by a hospital. 2 Reference Group. * Comparison with reference group is statistically significant at p <.05. Source: HSC Community Tracking Study Physician Survey, 2001 |
||||||
Practice Size Matters
There is significant variation in the availability of information technology across practice settings. The almost 70 percent of physicians in traditional settings—solo, small groups with up to 50 physicians or practices owned by hospitals4—were least likely to be in practices using information technology, with IT adoption rates ranging between 8 percent and 50 percent for the five functions examined. For most ofthe functions, physicians in large groups of more than 50 physicians and medical school faculty practices were about 50 percent more likely to report IT availability in the various patient support functions, compared with physicians in traditional practice settings. And, physicians practicing in staff- or group-model HMOs were more than twice as likely as those in traditional practice settings to have IT support for patient care.
Physicians in traditional practice settings were even less likely to be in practices with IT support for multiple functions (see Supplementary Table 1). Just 7 percent of physicians in small practices reported having IT support for four or five of the functions examined, compared with 20 percent of physicians in large groups and medical schools and more than 50 percent of those in staff/group HMOs.
Readier access to capital and administrative support staff, the ability to spread acquisition and implementation costs among more physicians, and active physician leadership may explain why larger practices are more likely to adopt IT to support patient care. In addition, large groups and HMOs offer greater opportunities and incentives for quality and efficiency gains such as improved care coordination from IT. However, IT support for patient care in medical school faculty practices, hospitalbased practices and large practices may be relatively more difficult to implement than in staff/group HMOs because of more complex governing structures, competing interests and a fluctuating patient base. Since staff/group HMO practices are integrated with insurance, they can capture the benefits of IT investment that typically go to insurers.
Back to Top
Other Factors Play Minor Role
Other factors such as physician age, specialty, and whether the practice is in an urban or rural area play relatively minor roles as underlying drivers of IT adoption. Older physicians were less likely than younger physicians to have IT support in their practices for all of the clinical functions except generating treatment reminders. Rates of IT adoption also differed between primary care physicians and specialists. Primary care physicians and specialists. Primary care physicians reported higher rates of adoption of technology to generate treatment reminders and prescribe electronically, while specialists had higher rates of adopting technology to exchange clinical data and access patient notes. Multivariate analysis shows that practice setting is, however, by far the most important driver of IT adoption of the factors examined (see Supplementary Table 2 for multivariate analysis).
Some policy makers have proposed focusing special efforts on speeding IT development in rural communities, given expectations that IT is likely to diffuse more slowly in those areas. For the most part, however, physicians in nonmetropolitan areas were just as likely as those in metropolitan areas to report that their practice had access to IT support, despite the fact that physicians in nonmetropolitan areas are more likely to be in smaller practices.5 The estimates for metropolitan and nonmetropolitan physicians were not significantly different from one another for any of the patient care functions except clinical data exchange, and metropolitan/nonmetropolitan differences for the proportion of physicians in practices with limited IT support (IT in zero or only one function) were also not statistically significant.
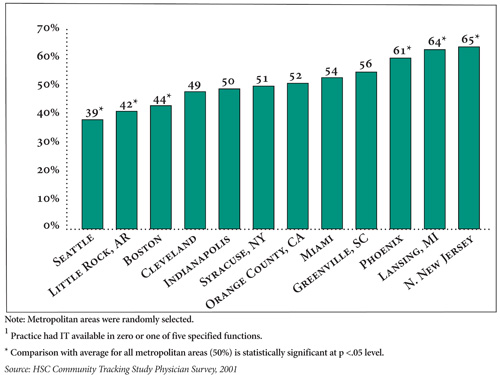
Although differences between urban and rural areas are not large, there is considerable variation in the availability of IT across the 12 metropolitan CTS communities. For example, more than 60 percent of physicians in three markets—Phoenix, Lansing and northern New Jersey—had limited access to IT support for patient care (IT in no more than one function), compared with less than 45 percent in Boston, Little Rock and Seattle (see Figure 2). These market differences remained after accounting for factors such as practice setting and physician age and specialty, suggesting other factors are driving variation across communities.
Back to Top
Figure 2 |
 |
Policy Options
Because barriers to IT adoption appear to be greatest for smaller traditional physician practices, policy makers may need to design policies specifically aimed at these physicians. While some of the approaches to speed IT adoption, particularly those addressing financial barriers, may provide incentives for smaller practices, others areless likely to be successful, especially in the near term.
Direct grants or loans to acquire IT and strategies to lower the costs of IT are two examples of approaches that may be more successful with smaller practices. For example, some advocates have encouraged the development of a government-sponsored funding mechanism to help provide capital to physicians and other providers akin to the Hill-Burton Act that permitted significant hospital expansion.6 WellPoint Networks Inc. and other health plans have implemented programs to give computer equipment or other IT support to physicians. The American Academy of Family Physicians’ electronic medical record initiative offers a relatively inexpensive “mini-electronic record,” coupled with organizational discounts, to reduce costs to smaller physician practices.7 Some state and local governments and private entities (primarily foundations and local health care providers), with some additional support from U.S. Department of Health and Human Services, are funding community data exchange initiatives that make patient information available to physicians over the Internet, minimizing costs for individual practices.
Other proposals may be less effective in promoting adoption in traditional practice settings. There are a number of health plan and purchaser initiatives underway to provide financial incentives to physicians to improve quality in their practices, and similar proposals are under review for Medicare. While some programs have explicit IT incentives, those that focus on performance targets offer only indirect motivation—adopting IT may improve the practice’s ability to meet the quality targets. Such quality initiatives are unlikely to address the financial barriers to IT adoption for smaller practices. IT investments typically must be made up-front, while incentive payments from a given quality initiative program are small, accrue incrementally on a per-patient basis, and apply to a limited portion of a practice’s patient base. In fact, until major health plans or Medicare offer practices significant financial incentives, quality initiatives are not likely to stimulate substantial IT adoption in smaller practices.
Back to Top
Notes
| 1. | Institute of Medicine, Crossing the Quality Chasm, National Academy Press, Washington, D.C. (2001). |
| 2. | U.S. Department of Health and Human Services, The Decade of Health Information Technology: Delivering Consumer-centric and Information-rich Health Care, Framework for Strategic Action, Washington, D.C. (July 21, 2004). |
| 3. | See, for example, e-Health Initiatives April 14, 2004, report indicating between 5 percent and 18 percent of physicians and other clinicians use electronic prescribing. The 2001 CTS estimate of 11 percent is well within this range. Report accessed June 24, 2004, at http://www.ehealthinitiative.org/initiatives/erx/document.aspx?Categ ory=249&Document=270. |
| 4. | While there is anecdotal evidence that some large hospital systems have been instrumental in providing IT for doctors in practices owned by the system, national rates of IT adoption to support patient care in practices owned by hospitals are similar to those in other traditional office-based practices. |
| 5. | Because of survey sample sizes in rural areas, it is not possible to determine if physicians in more remote rural areas are less likely to be in practices with IT than other physicians in nonmetropolitan areas. |
| 6. | Broder, Caroline, “Funding Health Care IT: Interview with Molly Coye,” i-HealthBeat, (Aug. 6, 2003.) Accessed June 1, 2004, at http://ihealthbeat.org/ index.cfm?Action=dspItem&itemID=99 805. |
| 7. | Chambliss, M.L, et al., “The Mini-electronic Medical Record: A Low-cost, Low-risk Partial Solution,” Journal of Family Practice (December 2001). |
Back to Top
Data Source
This Issue Brief presents findings from the HSC Community Tracking Study Physician Survey, a nationally representative telephone survey of physicians involved in direct patient care in the continental United States conducted in 2000- 01. The sample of physicians was drawn from the American Medical Association from the American Medical Association and the American Osteopathic Association master files and included active, nonfederal, office- and hospital- based physicians who spent at least 20 hours a week in direct patient care. Residents and fellows were excluded. The survey contains information on approximately 12,400 physicians. The response rate was 59 percent.
The CTS data suggest an upper limit on the number of physicians who regularly used IT to support patient care in 2001. The survey asked whether IT is available in the physician’s practice but did not measure how many physicians actually use IT or the frequency or intensity of their use. Moreover, the survey did not assess the sophistication of the systems being used. For example, physicians who use IT to access patient notes may have basic patient information in electronic form but not complete medical records. Furthermore, individual IT functions may not be designed to communicate readily with one another, and thus those practices with more functions with IT support do not necessarily have integrated clinical IT systems.
Back to Top
Supplementary Tables
Supplementary Table 1: Physicians
in Practices with Limited and Higher Levels of IT Support for Patient Care Functions
in 2001, by Practice and Physician Characteristics
Supplementary Table 2: Results
of Logistic Analysis: Odds Ratios for Factors Associated with Limited IT Support
for Patient Care Functions in Physicians’ Offices in 2001
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org
Vice President: Len M. Nichols