
Public Health Workforce Shortages Imperil Nation's Health
HSC Research Brief No. 4
April 16, 2008
Debra A. Draper, Robert E. Hurley, Johanna Lauer
After the 9/11 terrorist attacks, interest in the state of America’s public health system spiked, especially related to emergency preparedness. Significant new federal funding flowed to state and local agencies to bolster public health activities. But the spotlight on shoring up the nation’s public health system has faded, and the public appears unaware of escalating threats to such basic services as disease surveillance. Local health departments face a mounting workforce crisis as they struggle to recruit, train and retain qualified workers to meet their communities’ needs, according to a new study by the Center for Studying Health System Change (HSC).
Factors influencing the workforce shortage include inadequate funding, uncompetitive salaries and benefits, an exodus of retiring workers, insufficient supply of trained workers, and lack of enthusiasm for public health as a career choice. Local public health agencies have pursued strategies to improve workforce monitoring and planning, recruitment, retention, development and training, and academic linkages. However, little progress has been made to alleviate the shortages. Without additional support to address workforce issues, including the recruitment of the next generation of public health leaders, it is unlikely that local public health agencies will succeed in meeting growing community need, a situation potentially imperiling the public’s health.
- Public Health Workforce Crisis
- Nature of Shortages
- Factors Behind Shortages
- Community Responses
- Implications
- Notes
- Data Source
Public Health Workforce Crisis
![]() ess than 3 percent of the more than $2 trillion spent annually
on U.S. health care goes to government public health programs.1
Given the low priority placed on financing public health, it is hardly surprising
that substantial shortages of key public health workers plague local communities,
threatening basic services. Without enough skilled workers, public health agencies
are struggling to meet key responsibilities, including:
ess than 3 percent of the more than $2 trillion spent annually
on U.S. health care goes to government public health programs.1
Given the low priority placed on financing public health, it is hardly surprising
that substantial shortages of key public health workers plague local communities,
threatening basic services. Without enough skilled workers, public health agencies
are struggling to meet key responsibilities, including:
- Preventing the spread of disease;
- Protecting against environmental hazards;
- Reducing injuries;
- Promoting healthy behaviors; and
- Responding to disasters and assisting communities in recovery.2
What is surprising is the limited concern and awareness among the general public about these shortages and what they mean for public health agencies’ ability to provide essential services to safeguard the public’s health (see box below). This is well documented in recent research and vividly revealed by a persistent and pervasive underinvestment in public health.3 To examine the extent of public health workforce shortages, their causes and consequences, and strategies to address them, this study uses a community-based perspective, which included interviews of public health officials and other knowledgeable respondents in six communities: Cleveland; Greenville, S.C.; Indianapolis; Little Rock, Ark.; Orange County, Calif.; and Phoenix (see Data Source). Understanding the issues within a community context is particularly useful in assessing local priority placed on public health programs, investments in public health services, the available supply of public health workers and the degree of competition for skilled health professionals.
Experts have difficulty agreeing on the extent of the shortage. Since the release of the Institute of Medicine’s report on the “Future of Public Health” in 1988, various attempts have been made to enumerate the public health workforce and document shortages.4 However, the diverse nature of the occupations under the public health umbrella, coupled with a lack of agreement about which occupations constitute the field and whether the scope should be government only or more broadly inclusive, have led to significant variation in quantifying the workforce.5
Notwithstanding enumeration concerns, several organizations have conducted research to better understand the degree to which the supply of public health workers meets the demand, as well as which occupations have the greatest shortages. The National Association of County & City Health Officials (NACCHO) reported local health departments have the most difficulty recruiting public health nurses, epidemiologists and environmental health scientists or specialists.6 While the Health Resources and Services Administration’s (HRSA) 2005 public health workforce study found that budget constraints were the single biggest barrier to hiring public health workers, other factors posed important barriers, including general shortages of public health workers, uncompetitive salaries, and lengthy processing time for new hires.7 NACCHO also found uncompetitive salaries and benefits to be the primary drivers of local public health workforce shortages.8 And the Association of State and Territorial Health Officials (ASTHO) identified a rapidly aging workforce, chronic shortages of disciplines, such as nursing and epidemiology, and high turnover rates affected workforce trends.9 In addition, a number of studies and organizations have identified concerns about the adequacy of public health workers’ training and professional development opportunities.10
In analyzing the local public health workforce, it is important to recognize that different structural models are used to provide local public health services. In some communities, such as Little Rock and Greenville, local public health workers are state employees. In “home rule” states, local jurisdictions are responsible for public health, including counties such as Marion (Indianapolis), Orange (California), and Maricopa (Phoenix) or multiple municipalities (Cleveland metropolitan area). In still other communities, public health services are provided by a mix of local and state personnel.
Back to Top
Nature of Shortages
![]() tudy respondents were asked to identify shortages of professional personnel in terms of vacant positions, including positions that they were currently recruiting, and those they were unable to fill because of budget or other constraints. They also were asked to describe skill sets to perform core functions for which the required competencies were unavailable in their agencies. Shortages of critical personnel and deficits in key skill areas ranged from significant to severe across public health agencies in each of the six communities, with general agreement that public health nurses are the most difficult personnel to recruit and retain. Given the intense competition for nurses in general, public health agencies often are unable to recruit candidates, and nurses with bachelor’s degrees and specific training in public health are in particularly short supply. Nursing positions in some agencies remain vacant for many months; an average of six months was reported in Greenville, for example.
tudy respondents were asked to identify shortages of professional personnel in terms of vacant positions, including positions that they were currently recruiting, and those they were unable to fill because of budget or other constraints. They also were asked to describe skill sets to perform core functions for which the required competencies were unavailable in their agencies. Shortages of critical personnel and deficits in key skill areas ranged from significant to severe across public health agencies in each of the six communities, with general agreement that public health nurses are the most difficult personnel to recruit and retain. Given the intense competition for nurses in general, public health agencies often are unable to recruit candidates, and nurses with bachelor’s degrees and specific training in public health are in particularly short supply. Nursing positions in some agencies remain vacant for many months; an average of six months was reported in Greenville, for example.
In some communities with public health laboratories, such as Greenville, Orange County and Phoenix, agencies have difficulty hiring and retaining microbiologists and laboratory technicians. In Little Rock and Orange County, where local health departments also provide medical care, pharmacists and physicians reportedly are reluctant to work for the government for a variety of reasons, including low salaries. In most communities, local health departments also struggle to recruit and retain epidemiologists, sanitarians, clerical staff and information technology specialists.
In addition, agencies are wrestling with an overall lack of formal orientation to public health among workers, and in some cases, deficits in core public health skills. A remarkably small number of public health workers have received a basic introduction to public health beyond their immediate job functions. In Little Rock, for example, individuals with graduate public health degrees are rare and in high demand. In Indianapolis, one respondent noted that, “We have people who are doing epidemiology field work, but they’ve never been educated in epidemiology. They are getting on-the-job training, if you will.”
Moreover, many local health departments lack workers with key leadership and management skills. As one respondent observed, “People are promoted from a clinical role to a managerial role when they do a good job in the clinical role, but they do not necessarily have managerial training or education of any sort.” Although these skill deficits are not always identified in workforce surveys, they significantly impact the ability of public health agencies to provide effective services.
Public health officials in Little Rock and Greenville also were concerned with the long-term ramifications of the shortages and skill deficits. Without qualified, core public health workers, officials were concerned about their ability to respond in a crisis or to pursue population-based strategies, such as health promotion. In Phoenix, for example, limited funding and lack of workers severely hampered routine surveillance activities, resulting in at least one untoward event—a salmonella outbreak at an Arizona orange juice plant that was not identified until the juice reached Washington state and officials there identified the outbreak.
Local health departments sometimes have opted, although reluctantly, to outsource critical functions. For example, a Cleveland area health department contracts with a local hospital to obtain physician services and occasionally outsources epidemiology and biostatistics functions to a local university. Similarly, Indianapolis and Orange County health officials have resorted to contracting with temporary nursing agencies. However, other local health departments have been reticent to do this because of the significant costs involved and because most agency nurses have no public health training.
Back to Top
Factors Behind Shortages
![]() espondents identified several key factors influencing public health workforce shortages. While local public health agencies have grappled with many of these factors for some time, respondents reported problems are worsening. The key factors discussed include:
espondents identified several key factors influencing public health workforce shortages. While local public health agencies have grappled with many of these factors for some time, respondents reported problems are worsening. The key factors discussed include:
- Inadequate public health funding;
- Uncompetitive salaries and benefits;
- Looming exodus of retiring workers;
- Insufficient supply of trained workers; and
- Lack of enthusiasm for public health careers.
Inadequate Funding
Universally, respondents described public health funding as inadequate, undermining public health agencies’ ability to recruit and retain a sufficient and trained workforce. As an Arkansas public health official said, “It’s not that we have the money, but can’t find the people. It’s that we don’t have the money to even begin to find the people. Our issues are linked to the insufficiency of investment in public health generally.”
Many local public health departments have benefited since 9/11 from increased federal funding for emergency preparedness activities. These funds have reportedly helped with workforce recruitment and staff development, but respondents said funding is declining, and much less predictable. An Ohio public health official described the difficulty, “When you have a [job] candidate sitting in your office, you have to say, ‘I don’t know what the funding will look like. If the funding goes, you go.’”
Adequate funding is a particular problem in communities with significant demographic changes, including growing ethnic and cultural diversity and, in some cases, growing populations. A Phoenix public health official said, “Our services haven’t grown in size with the rapidly growing population. Our population increased by 100,000 per year for the last couple of decades, and you look back and programs are still the same size as a couple of decades ago, even simple services like vital records. Our staffing is just nowhere close to keeping up with demand.”
Many respondents attributed inadequate funding to the general lack of political support for public health. A common theme was that public health is “just not a priority for our legislature.” As an Arizona respondent noted, “The Legislature doesn’t understand the importance of education or health, and especially not public health. We try to do a lot of work around educating our legislators about what public health is and why it’s important. But we have a high turnover in our Legislature, so it’s a constant education battle.” Further, public health in local communities usually competes with fire and police for funding, and respondents said these areas are a higher priority.
Uncompetitive Compensation
Funding difficulties preclude most local public health agencies from effectively competing with other organizations, often private, that are seeking workers with similar training and skills. Uncompetitive salaries were the most frequently cited reason for being unable to attract candidates to public health, especially new graduates who face large student loans.
Respondents said the competition is most acute for nurses because acute-care hospitals pay much higher salaries—sometimes as much as $15,000 or $20,000 more. Sign-on bonuses of $10,000 or more often are used to lure nurses to the private sector, a strategy most public health agencies cannot match. Respondents noted such a high demand for nurses that they essentially “can walk out one door and immediately work for somebody else.” An Orange County respondent described the impact: “In the last two years, I’ve seen close to a dozen nurses who left public health to go back and do clinical work because they can get paid so much more. We have never paid those folks what they gain in the private sector, but we provide them with other benefits, better pensions, better work hours. So, it’s kind of equilibrated. But when the difference is very large, then it becomes impossible.”
The salary issues, however, are not exclusive to nurses. Other positions—generally those requiring advanced training and education—also are affected. Respondents reported that the insurance industry, biotechnology companies and universities generally pay epidemiologists much better. Nutritionists reportedly are paid better by acute-care hospitals in some communities. And laboratory scientists often are attracted to private laboratories that pay substantially higher salaries, which in Phoenix, for example, were estimated as 30 percent to 40 percent more.
In some communities, government agencies compete with one another for public health workers. Salaries are not always comparable between agencies because positions requiring the same skill set may be classified and paid differently from one agency to another. This sometimes occurs between state and local public health agencies, particularly when both agencies are located in the same community. In Phoenix, for example, the state reportedly pays epidemiologists $20,000 more than Maricopa County.
Although benefits and work schedules once provided advantages for public employers, heightened demand for workers has increasingly closed the gap as private employers have enriched benefits and developed more flexible scheduling. The one benefit that remains a key advantage for public health workers, however, is retiree health benefits. As private industry has moved away from offering these benefits, the ability to continue offering retiree health benefits remains an important differentiator for many public health agencies.
Inflexible government hiring and compensation systems reportedly are an additional impediment faced by local public health agencies. One respondent noted, “The bureaucracy of the local health department for both recruitment and advancement. has been an issue raised by folks in exit interviews. They said they couldn’t take the system. It didn’t matter if you did a good job or not. There is no way of establishing yourself for outstanding service. You just do what is expected of you.”
Exodus of Retiring Workers
Across the six communities, respondents discussed public health’s “silent crisis”—the aging of the public health workforce and the looming exodus of workers eligible for retirement. According to ASTHO’s 2007 survey, the average age of state public health workers is nearly 47 years, considerably higher than the average age of the workforce generally.11 As a respondent of one national public health organization noted, “It’s not something that will make the front page of the paper, but if we don’t do something to address it better than we are now, we will feel the effects in the near term.”
ASTHO’s 2007 survey also found that by 2012, 50 percent of some state health agencies’ workforces will be eligible to retire.12 In South Carolina, for example, estimates show 60 percent of the statewide public health workforce is aged 44 or older. In Ohio, at least half of the state’s 130 health commissioners are expected to retire in the next 10 to 15 years. Phoenix was the sole exception to this pattern, as officials reported a comparatively younger workforce, reflecting the area’s demographics and rapid population growth.
Respondents discussed that most public health agencies do not have good succession plans in place and, as a result, retirements will likely intensify workforce shortages. Public health officials said that they were most concerned about ensuring the transfer of important institutional knowledge from retiring workers to new workers. They also discussed concerns about the loss of mentoring and other collegial relationships as key staff members retire. But some respondents also discussed opportunities, noting that retirements can establish a platform for change—change that otherwise might be difficult to accomplish, particularly if long-time staff is resistant. Retirements also can provide an opportunity to lower costs by replacing more expensive tenured staff with less expensive new staff.
Insufficient Trained Workers
Across communities, an insufficient supply of trained public health workers has reportedly contributed to workforce shortages, especially for public health nurses. The nursing shortage is not exclusive to public health. More nurses are aging out of the workforce, the demand continues to exceed supply, and training capacity is constrained in large part because of a nursing faculty shortage.13
In addition to nurses, there are shortages of other workers with advanced degrees and public health training. While respondents acknowledged there are more schools of public health and training programs than existed a decade or so ago, most graduates—reportedly 80 percent—do not end up in the public sector. An Indiana respondent said, “It’s discouraging to graduate these well-prepared master’s folks and then for them not to go into public health departments.”
Respondents reported that public health workers increasingly need more specialized skills, adding to recruitment challenges. For example, respondents across communities reported a critical shortage of workers with bilingual skills. As an Arizona respondent said, “There just aren’t enough bilingual professionals. So many of the people who are front-line workers are without formal training and are just thrown into the position of having to be interpreters of the language and cultural behavior. It’s not a good situation.”
Shortage issues are similar for workers with management and leadership skills. A number of contemporary public health issues have brought new, unfamiliar responsibilities to public health managers. Respondents also expressed particular concern about the leadership vacuum that the impending wave of retirements is likely to create.
Lack of Enthusiasm for Public Health Careers
Respondents echoed a common sentiment about the need to generate enthusiasm for public health as a career. As an Ohio public health official suggested, “Most people come to public health because they fall into it, not because it was presented as a great career opportunity.” Respondents decried that not enough young people are attracted to public health. According to a representative of a national public health organization, “There’s not in the younger generation the same sort of perception that government is an interesting job. My former supervisor used to say that nobody says, ‘Come be a pointy-headed bureaucrat.’ That’s not an attractive sell to the younger generation.”
In part, the lack of enthusiasm for public health careers is attributed to the absence of a clear career path for many positions. Opportunities for advancement are limited, which respondents said is particularly unappealing to young people and discourages them from pursuing these careers. For those already employed in public health, poor advancement opportunities reportedly contribute to turnover, especially in areas where competition is strong for workers with more specialized skills. Public health workers also have few incentives to obtain additional training through a graduate public health program, for example, to improve their knowledge and skills. As a Little Rock public health official said, “If it doesn’t bring you more money or advancement, there is a sense that there is no sense in doing it.”
Respondents also discussed the increasing stress—particularly since 9/11—associated with the public health work environment that makes recruitment and retention more difficult. As an Arkansas public health official said, “Many people came to public health for more predictable hours and a limited scope of responsibility, but increasingly since 9/11, especially, we see public health as a 24/7 responsibility in terms of emergency response and emergency preparedness.” Respondents described the increased stress as also stemming from workers being asked to do more with fewer resources, assuming larger caseloads, and trying to manage demanding federal grant requirements.
Back to Top
Community Responses
![]() espondents discussed several important strategies to respond to shortages of public health workers. But in many communities, the ability of local public health agencies to respond is severely constrained by such factors as the lack of funding. The key strategies that local public health agencies reported pursuing include:
espondents discussed several important strategies to respond to shortages of public health workers. But in many communities, the ability of local public health agencies to respond is severely constrained by such factors as the lack of funding. The key strategies that local public health agencies reported pursuing include:
- Monitoring and planning;
- Recruitment;
- Retention;
- Workforce development and training;
- Academic linkages; and
- Racial, ethnic and linguistic diversity.
Monitoring and Planning
Assessment of worker shortages and planning varied across communities. Few public health agencies had extensively studied the “pipeline” for workers, but in South Carolina concerns about impending retirements and persistent recruitment problems in key occupational areas triggered a systematic study of shortages in 2004. The findings set in motion several actions, including a multi-faceted recruitment plan and a detailed design for workforce training.
Personnel shortages also were addressed in a 2004 study of public health in Indiana that noted the state’s low ranking in a national survey of public health personnel-to-population ratios. Other communities rely heavily on anecdotal evidence, observations, and specific recruitment difficulties—such as for nurses in Orange County—to stimulate plans. In some states and communities, public health officials have pooled efforts with other public agencies to develop interagency strategies to address shortages.
Recruitment
Since salary issues are the primary recruitment barrier, considerable attention has focused on devising strategies to address these concerns. In several communities, public health agencies have sought and received salary upgrades for key clinical staff or administrative discretion to make adjustments. One public health official emphasized that because of serious shortages, “I had to raise my salaries to be competitive [otherwise] it was very difficult for us to carry out our mandate.” Arkansas devised a system that includes additional pay for experience and education to enable nurse salaries to be more competitive. South Carolina has made across-the-board salary adjustments for some clinical positions and selectively uses signing bonuses. Yet, there is a downside to raising salaries. As an Arizona public health official noted, “In just the three years since I’ve been here, our nursing salaries have gone up 30 percent. When we were level grant funded, and you have nurses on those grant dollars, that just kills the grants and it’s part of the financial reality. The cost of just keeping what we had was going up substantially.”
Different strategies were used to specifically deal with nursing recruitment challenges. Orange County assigned a senior nurse to be a full-time nurse recruiter to address shortages, particularly in public health and corrections, that had been exacerbated by mandatory staffing ratios in California hospitals. Some public health agencies addressed persistent recruitment problems in Arizona by reducing the demand for registered nurses through job redesign or narrowing requisite skill levels to be more selective in what tasks these positions were assigned. Other agencies aspired to “recreate public health nursing” by limiting hires only to bachelor’s degree nurses because associate’s degree nurses lack sufficient community health training.
Several local agencies noted expanded efforts to reach potential hires earlier in their career choice processes and to cultivate a positive perception of public health. This includes information campaigns, high school and college visits, and internship and shadowing opportunities. A number of respondents noted the different expectations of younger workers about the pace of career advancement and long-term commitments to public-sector employment. One observer suggested that this generation lacks the “sense that ‘I’m going to work my way up.’”
Retention
As with recruitment, salary disparities present key challenges for public health agencies in retaining valued staff and responding to competition from private-sector employers or, in some cases, other public organizations. Adjustments to salary schedules were widely used, especially for nurses where mobility is greatest. Retention bonuses were used in South Carolina, Indianapolis and Orange County. Laboratory technicians and sanitarians presented special challenges because of their attractiveness to private-sector employers upon completion of their public health training.
Educational opportunities, including tuition reimbursement, release time and financial rewards for obtaining advanced degrees are particularly valuable for public health workers. Allowing nurses to develop a more specialized focus on a specific professional interest is used in Indianapolis to promote development of clinical personnel.
The impact of retirements was a prominent concern, though respondents generally agreed “the massive wave of retirees hasn’t quite hit.” Impending retirements have shifted attention to instituting more formal mentoring, shadowing and job rotation programs. Respondents in Orange County noted concerns given the seniority of its top echelon of executives and bolstered its management development program. But a national respondent suggested that there is not “the sense of urgency for succession planning in public health and civil service” that is seen in private business.
Development and Training
Because financial constraints preclude hiring substantial numbers of new personnel, most public health departments acknowledged the need for more investment in workforce development and training. Linkages to academic institutions represent a key piece of these efforts, but most respondents identified even more basic needs, given that so few workers have received any formal training in public health and many only have skills acquired on the job. The Arkansas Public Health Institute was developed in partnership with the University of Arkansas for Medical Sciences School of Public Health to train existing workers, many of whom lack more formal education in public health. Because funding for training has been neglected in the past, many agencies had huge backlogs of the most basic training needs.
The core competencies promulgated by the Council on Linkages, a joint initiative of organizations representing public health practitioners and academics, were repeatedly cited as playing an instrumental role in identifying needed skills, articulating training needs, and shaping new training opportunities. The post-9/11 focus on emergency preparedness has stimulated much more attention to training needs, provided new resources to carry this out, and forged new relationships between public health officials and other entities. One noted example was that communication-related investments in local health departments now make online/distance education programs more readily available at local worksites. At the same time, some respondents believed that a disproportionate emphasis on emergency preparedness comes at the expense of other areas needing at least as much, if not more, training and development. Beyond these specific concerns, there is also significant debate on the value of the nascent movement to implement a certification program for public health workers.
Leadership and management training is a key priority in most agencies. Respondents in Cleveland touted the Ohio Health Commissioner’s Academy as illustrative of the value in starting training efforts at the very top of the agency. Likewise, each community reported positive experiences with participation in the management institutes funded by HRSA at selected schools of public health around the country. Several respondents cited the need to develop mechanisms that institutionalize and reinforce training initiatives so that advancement is conditioned on successful participation in professional development opportunities.
Academic Linkages
Schools and programs in public health have the potential to help address local workforce needs, and their roles are prominent in most of the communities. The new school of public health in Little Rock is a particularly good example, focusing on training a new cadre of professionals and providing substantial development and training to existing public health employees. The University of South Carolina plays a comparable role for the state public health agency and is implementing continuing education and graduate certificate courses as part of a major statewide staff development program. Graduate public health programs in Cleveland and Indianapolis offer related initiatives on a smaller scale, and programs in development in Orange County have similar aspirations.
Several respondents cited positive experiences with the HRSA-funded public health institutes despite the relatively small size and limited support the programs have received. “When adequately funded, HRSA’s program has been phenomenal,” one national respondent commented, “but it has not been funded real well.” In particular, these programs enable agencies to infuse public health competencies and values into training initiatives, and their embrace of distance learning enables local departments to expand participation dramatically, particularly for workers in outlying areas. Leadership training was seen as particularly valuable because of its focus on instilling stronger skills in business plan development and implementation.
Racial, Ethnic Diversity
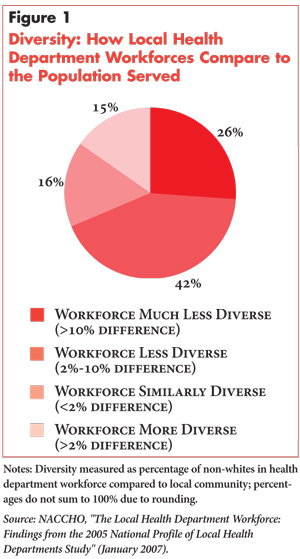
While a goal of public health agencies is to ensure their workers “look like” the communities they serve, this reportedly has been difficult to achieve. As NACCHO found in 2005, it is more often the case that the workforces of local public health departments are less diverse than the populations they serve (see Figure 1).14
A number of officials commented on the importance of promoting more racial, ethnic and linguistic diversity in their workforce. Others contended, however, that the priority should be cultural competency. Still others said shortages of key personnel are so acute that minority hiring is a secondary concern. One respondent noted, “We want to be as diverse as possible, but when you have limited pools, you have a more difficult time.” In addition, inflexibility in hiring practices and diminished priority of affirmative action are reportedly added impediments. In light of these concerns, many respondents indicated the need to intensify efforts to develop career ladders and advancement opportunities for minorities already employed in public health.
Back to Top
Implications
![]() everal key conclusions can be drawn from this community-based perspective on public health workforce shortages:
everal key conclusions can be drawn from this community-based perspective on public health workforce shortages:
- Shortages are likely to persist and to worsen given aggressive competition from the private sector and overall scarcity of key health professionals.
- Skill deficits are less apparent than worker shortages but may be more consequential in adversely affecting the quantity and quality of public health services.
- Since infusion of substantial funds for new hiring is unlikely in the near term, investments in the development, training and retention of existing workers are critical.
- Relationships with academic public health programs have value and promise, but are typically underdeveloped and require more focused attention to be mutually rewarding.
- Changing of the guard to the next generation of public health workers and leaders presents key opportunities if adequately anticipated and planned.
Studying public health workforce shortages at the community level brings into focus the extent to which communities are under-investing in an area that has critical, but inadequately recognized, consequences. All six of the communities have highly regarded health care providers, including widely recognized hospital systems that have succeeded in obtaining the necessary workers and skill sets to serve their communities’ needs. Even the publicly owned or sponsored acute-care providers in these communities have found the resources to secure an adequate workforce despite serious supply problems. That, however, has not been the case for public health agencies.
Instead, communities have chosen to forgo what would be seen as essential services in many locales. They face delays in getting basic services or having them provided by persons with questionable qualifications. They routinely accept greater risks of health problems arising because of insufficient surveillance or inadequately trained workers. They also may lack the leadership needed to take charge and provide direction in the event of a serious public health crisis. All of these problems will likely worsen as recruitment difficulties persist, retention challenges grow and the wave of approaching retirements crests.
Noteworthy efforts are underway in some communities to alter this trajectory. But absent greater public awareness of the shortages and their consequences, with a corresponding increase in a commitment of resources to address them, the contemporary public health system cannot adequately attend to the health of the nation.
Back to Top
Notes
Back to Top
Data Source
Public health workforce issues and the strategies used to recruit, retain and develop public health workers were studied in six communities: Cleveland; Greenville, S.C.; Indianapolis; Little Rock, Ark.; Orange County, Calif.; and Phoenix. These six communities are from the Community Tracking Study (CTS) and were selected based on preliminary findings from the 2007 CTS site visits as having focused, at least to some degree, on their public health workforce needs. A total of 46 interviews were conducted between November 2007 and January 2008. The majority of the interviews were conducted with representatives of state and local public health agencies, state public health associations, public health academic training programs, and other knowledgeable observers. Representatives of key national public health organizations also were interviewed to obtain additional insights and perspectives. A two-person research team conducted each interview, and notes were transcribed and jointly reviewed for quality and validation purposes. All interview data were coded and analyzed using Atlas.ti, a qualitative software package.
Back to Top
Acknowledgement: This research was supported under a grant from a special solicitation for Public Health Systems Research throught the Robert Wood Johnson Foundation’s Health Care Financing and Organization Initiative, which is administered by AcademyHealth.
ISSUE BRIEFS are published by the
Center for Studying Health System Change.
600 Maryland Avenue, SW, Suite 550
Washington, DC 20024-2512
Tel: (202) 484-5261
Fax: (202) 484-9258
www.hschange.org