Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


Highly Consolidated Market Poses Cost Control Challenges
Lansing, Mich.
Community Report No. 06
Winter 2001
Kelly Devers, Jon B. Christianson, Laurie E. Felland, Suzanne Felt-Lisk, Liza Rudell, J. Lee Hargraves
 n October 2000, a team of researchers visited Lansing, Mich.,
to study that community’s health system, how it is changing and the effects of
those changes on consumers. The Center for Studying Health System Change (HSC),
as part of the Community Tracking Study, interviewed more than 85 leaders in the
health care market. Lansing is one of 12 communities tracked by HSC every two
years through site visits and surveys. Individual community reports are published
for each round of site visits. The first two site visits to Lansing, in 1996 and
1998, provided baseline and initial trend information against which changes are
tracked. The Lansing market includes Ingham, Clinton and Eaton counties. n October 2000, a team of researchers visited Lansing, Mich.,
to study that community’s health system, how it is changing and the effects of
those changes on consumers. The Center for Studying Health System Change (HSC),
as part of the Community Tracking Study, interviewed more than 85 leaders in the
health care market. Lansing is one of 12 communities tracked by HSC every two
years through site visits and surveys. Individual community reports are published
for each round of site visits. The first two site visits to Lansing, in 1996 and
1998, provided baseline and initial trend information against which changes are
tracked. The Lansing market includes Ingham, Clinton and Eaton counties.
One health plan and one hospital system now control much of Lansing’s health care
market. Blue Cross and Blue Shield of Michigan (BCBSM), the dominant plan, covers
about 70 percent of commercially insured individuals. The dominant hospital system,
Sparrow Health System, which was created by the merger of two local hospitals
in 1997, now controls more than 60 percent of the hospital market. It also owns
Lansing’s second major health plan, Physicians Health Plan of Mid-Michigan (PHP).
Recent developments suggest that controlling health
care costs in Lansing’s highly consolidated market may be
challenging. Since 1998, employers have been hit with double-digit
health plan premium increases and have responded
only modestly. Other important developments include:
- Hospitals have expanded some clinical services and have
negotiated payment increases from health plans.
- Controversies over freestanding ambulatory surgery
centers (ASCs) have reignited.
- Physicians have adopted strategies to increase their
leverage with plans and hospitals.
- The county health department has continued to lead
efforts to improve care and coverage for the uninsured.
Hospitals Compete Aggressively in Certain Clinical Service Lines
 ince 1998, Lansing’s two hospital systems-
Sparrow Health System and the
Ingham Regional Medical Center (IRMC)-
have invested significant resources to
build new tertiary care facilities and to add
or expand clinical service lines. The
expansions are targeted at gaining community
recognition as the highest-quality,
"brand-name" hospital to build loyalty
and enhance profitability.
Sparrow, which had started a cardiovascular surgery program to compete with IRMC,
recently added a Level I trauma unit and a neurosurgical care unit. With an infusion
of capital from its parent organization, McLaren Health Care Corporation, IRMC
added a $21 million women and children’s center to compete with Sparrow in obstetrics/gynecology
and pediatrics to attract younger, middle-class families. IRMC also recently established
the Great Lakes Cancer Institute, a joint venture with Michigan State University
(MSU) to enhance cancer research, services and teaching programs. The arrangements
also will move MSU’s clinical faculty practice and oncology fellowship program
from Sparrow to IRMC. Sparrow has mounted an aggressive advertising campaign to
market its new and improved facilities and services to the community, and IRMC
is expected to launch similar efforts. According to respondents, Sparrow is now
regarded as the premier hospital in the community, but IRMC has advanced in recent
years to become a more formidable competitor.
The increased competition between
Sparrow and IRMC in clinical services
was viewed positively by most respondents,
with a few exceptions. Most of those interviewed
considered the new or enhanced
services valuable to the community,
noting that competition between the two
hospital systems extends to outreach, prevention
and charity care. On the other
hand, some respondents were concerned
about the long-term effects of service
competition on costs and access to more
basic services. ince 1998, Lansing’s two hospital systems-
Sparrow Health System and the
Ingham Regional Medical Center (IRMC)-
have invested significant resources to
build new tertiary care facilities and to add
or expand clinical service lines. The
expansions are targeted at gaining community
recognition as the highest-quality,
"brand-name" hospital to build loyalty
and enhance profitability.
Sparrow, which had started a cardiovascular surgery program to compete with IRMC,
recently added a Level I trauma unit and a neurosurgical care unit. With an infusion
of capital from its parent organization, McLaren Health Care Corporation, IRMC
added a $21 million women and children’s center to compete with Sparrow in obstetrics/gynecology
and pediatrics to attract younger, middle-class families. IRMC also recently established
the Great Lakes Cancer Institute, a joint venture with Michigan State University
(MSU) to enhance cancer research, services and teaching programs. The arrangements
also will move MSU’s clinical faculty practice and oncology fellowship program
from Sparrow to IRMC. Sparrow has mounted an aggressive advertising campaign to
market its new and improved facilities and services to the community, and IRMC
is expected to launch similar efforts. According to respondents, Sparrow is now
regarded as the premier hospital in the community, but IRMC has advanced in recent
years to become a more formidable competitor.
The increased competition between
Sparrow and IRMC in clinical services
was viewed positively by most respondents,
with a few exceptions. Most of those interviewed
considered the new or enhanced
services valuable to the community,
noting that competition between the two
hospital systems extends to outreach, prevention
and charity care. On the other
hand, some respondents were concerned
about the long-term effects of service
competition on costs and access to more
basic services.
Freestanding Ambulatory Surgery Centers Reignite Controversy
 hree freestanding ASCs were started by
physician entrepreneurs between 1996
and 1998, generating controversy over the
role of such ASCs in the provision of
ambulatory surgery services. A March 2000
ruling by Michigan’s state insurance commissioner
reignited that controversy.
The debate about whether to include
freestanding ASCs in commercial plan
networks illustrates the complex issues
raised by facilities that compete to provide
services traditionally provided by hospitals.
Proponents argue that freestanding
ASCs should be given the opportunity to
compete with hospital-based ASCs. More
specifically, they contend that, compared
with hospital-based ASCs, freestanding
ASCs have substantially lower costs and
higher consumer satisfaction and are of
equal or better quality.
Opponents argue that the freestanding
ASCs duplicate hospital capacity, ultimately
resulting in higher total costs. For
this reason, General Motors (GM) has
refused to allow plans serving its employees
to include freestanding ASCs in their networks.
In part because of GM’s position
on this issue, BCBSM also has refused to
contract with these entities. Over the past
two years, however, a successful lawsuit
filed by one of the local ASCs led BCBSM
to include it in its network, although
BCBSM subsequently raised concerns
about the quality of care the center provided,
given its low volume of procedures.
In March 2000, Michigan’s state
insurance commissioner ruled that
BCBSM’s refusal to contract with freestanding
ASCs was based on inequitable
access and quality standards. BCBSM’s
new standards, which may make it easier
for freestanding ASCs to participate in
BCBSM indemnity products, are currently
under review by the commissioner. If these
new criteria result in BCBSM expanding
its contracts with ASCs, the Lansing market
is likely to see increased competition
for ambulatory surgery services in the
years ahead, which will help test theories
of ASCs’ implications for cost, quality
and consumer satisfaction. hree freestanding ASCs were started by
physician entrepreneurs between 1996
and 1998, generating controversy over the
role of such ASCs in the provision of
ambulatory surgery services. A March 2000
ruling by Michigan’s state insurance commissioner
reignited that controversy.
The debate about whether to include
freestanding ASCs in commercial plan
networks illustrates the complex issues
raised by facilities that compete to provide
services traditionally provided by hospitals.
Proponents argue that freestanding
ASCs should be given the opportunity to
compete with hospital-based ASCs. More
specifically, they contend that, compared
with hospital-based ASCs, freestanding
ASCs have substantially lower costs and
higher consumer satisfaction and are of
equal or better quality.
Opponents argue that the freestanding
ASCs duplicate hospital capacity, ultimately
resulting in higher total costs. For
this reason, General Motors (GM) has
refused to allow plans serving its employees
to include freestanding ASCs in their networks.
In part because of GM’s position
on this issue, BCBSM also has refused to
contract with these entities. Over the past
two years, however, a successful lawsuit
filed by one of the local ASCs led BCBSM
to include it in its network, although
BCBSM subsequently raised concerns
about the quality of care the center provided,
given its low volume of procedures.
In March 2000, Michigan’s state
insurance commissioner ruled that
BCBSM’s refusal to contract with freestanding
ASCs was based on inequitable
access and quality standards. BCBSM’s
new standards, which may make it easier
for freestanding ASCs to participate in
BCBSM indemnity products, are currently
under review by the commissioner. If these
new criteria result in BCBSM expanding
its contracts with ASCs, the Lansing market
is likely to see increased competition
for ambulatory surgery services in the
years ahead, which will help test theories
of ASCs’ implications for cost, quality
and consumer satisfaction.
Physicians Move to Increase Leverage with Plans and Hospitals
 hysicians in Lansing’s highly consolidated
and increasingly competitive market have
relied on several strategies to maintain
their autonomy and increase their leverage
with plans and hospitals by: (1) consolidating
into larger practice groups; (2)
adopting a more aggressive negotiating
stance with plans; and (3) continuing
their participation in the physician-hospital
organizations (PHOs) of both Sparrow
and IRMC.
Although some larger physician
groups have formed in Lansing in past
years, small single-specialty groups have
been more successful recently in consolidating
than have larger ones. Over the
past two years, there have been a number
of instances in which specialists in solo
practices and very small groups have consolidated
into larger groups of approximately
10 physicians. Meanwhile, two of the three
larger physician groups that had been
growing-Thoracic and Cardiovascular
Institute and Mid-Michigan Physicians-
lost momentum in the drive to grow
because they had to focus on other management
issues related to declining Medicare
reimbursement and developing information
systems to support their practices.
Physician groups also have asserted
themselves recently by demanding changes
in their contracts with health plans. Having
found that extensive risk-sharing arrangements
with plans are unprofitable for
them, most physician groups have shown
little interest in capitated arrangements
(other than for primary care services)
with health plans. Several physician groups
have renegotiated or pulled out of the few
capitated contracts they had. In addition,
physicians have taken steps to improve
their fee-for-service contracts, securing
better contract terms and improved
payment rates.
Finally, physicians have improved
their position compared to local hospitals
as pressure to align exclusively with one
of the two hospitals’ PHOs has waned.
Because PHOs have not become the major
contracting vehicles in the market as anticipated,
hospitals have less leverage to push
for exclusive physician membership. As a
result, physicians have been successful in
maintaining relationships with both
Sparrow and IRMC’s PHOs, reducing
physicians’ dependence on any one hospital. hysicians in Lansing’s highly consolidated
and increasingly competitive market have
relied on several strategies to maintain
their autonomy and increase their leverage
with plans and hospitals by: (1) consolidating
into larger practice groups; (2)
adopting a more aggressive negotiating
stance with plans; and (3) continuing
their participation in the physician-hospital
organizations (PHOs) of both Sparrow
and IRMC.
Although some larger physician
groups have formed in Lansing in past
years, small single-specialty groups have
been more successful recently in consolidating
than have larger ones. Over the
past two years, there have been a number
of instances in which specialists in solo
practices and very small groups have consolidated
into larger groups of approximately
10 physicians. Meanwhile, two of the three
larger physician groups that had been
growing-Thoracic and Cardiovascular
Institute and Mid-Michigan Physicians-
lost momentum in the drive to grow
because they had to focus on other management
issues related to declining Medicare
reimbursement and developing information
systems to support their practices.
Physician groups also have asserted
themselves recently by demanding changes
in their contracts with health plans. Having
found that extensive risk-sharing arrangements
with plans are unprofitable for
them, most physician groups have shown
little interest in capitated arrangements
(other than for primary care services)
with health plans. Several physician groups
have renegotiated or pulled out of the few
capitated contracts they had. In addition,
physicians have taken steps to improve
their fee-for-service contracts, securing
better contract terms and improved
payment rates.
Finally, physicians have improved
their position compared to local hospitals
as pressure to align exclusively with one
of the two hospitals’ PHOs has waned.
Because PHOs have not become the major
contracting vehicles in the market as anticipated,
hospitals have less leverage to push
for exclusive physician membership. As a
result, physicians have been successful in
maintaining relationships with both
Sparrow and IRMC’s PHOs, reducing
physicians’ dependence on any one hospital.
Hospitals Negotiate Small Payment Increases from Plans
 aced with declining reimbursement
from Medicare and Medicaid and rapidly
rising costs, Lansing’s hospital systems
have pushed back on commercial health
plan contracts and finally secured small
payment increases after years of considerable
discounts.
Hospitals nationally have confronted
declining Medicare revenues under the
Balanced Budget Act (BBA) of 1997,
and as teaching institutions, Sparrow
and IRMC have experienced additional
declines because of the BBA’s provisions
regarding graduate medical education.
These problems have been compounded
by difficulties in Michigan’s Medicaid
managed care program, including payments
that providers allege are too low
and too slow. At the same time, hospitals
have experienced substantial cost increases
driven by labor shortages, pressure to
acquire new technologies and information
systems and rising inpatient pharmaceutical
costs.
Now that they are the only two hospital
systems, Sparrow and IRMC have
more leverage in their negotiations with
BCBSM and PHP, especially in an environment
where plans must include both
hospital systems in their products to be
successful. This leverage has enabled them
to negotiate higher payment rates from
health plans.
Another response to financial pressures
by Lansing’s hospital systems has been to
cut selected clinical and administrative
services and improve efficiency. IRMC, for
example, eliminated approximately 80
positions by consolidating administrative
functions with its parent organization and
discontinuing services, such as transitional
care units, that the hospital determined
were no longer reimbursed adequately
under Medicare.
Sparrow and IRMC also expect some
relief from financial pressures in the near
future, thanks to the recent restoration of
some Medicare BBA funds and increases
in provider reimbursement rates in
Michigan’s Medicaid managed care program. aced with declining reimbursement
from Medicare and Medicaid and rapidly
rising costs, Lansing’s hospital systems
have pushed back on commercial health
plan contracts and finally secured small
payment increases after years of considerable
discounts.
Hospitals nationally have confronted
declining Medicare revenues under the
Balanced Budget Act (BBA) of 1997,
and as teaching institutions, Sparrow
and IRMC have experienced additional
declines because of the BBA’s provisions
regarding graduate medical education.
These problems have been compounded
by difficulties in Michigan’s Medicaid
managed care program, including payments
that providers allege are too low
and too slow. At the same time, hospitals
have experienced substantial cost increases
driven by labor shortages, pressure to
acquire new technologies and information
systems and rising inpatient pharmaceutical
costs.
Now that they are the only two hospital
systems, Sparrow and IRMC have
more leverage in their negotiations with
BCBSM and PHP, especially in an environment
where plans must include both
hospital systems in their products to be
successful. This leverage has enabled them
to negotiate higher payment rates from
health plans.
Another response to financial pressures
by Lansing’s hospital systems has been to
cut selected clinical and administrative
services and improve efficiency. IRMC, for
example, eliminated approximately 80
positions by consolidating administrative
functions with its parent organization and
discontinuing services, such as transitional
care units, that the hospital determined
were no longer reimbursed adequately
under Medicare.
Sparrow and IRMC also expect some
relief from financial pressures in the near
future, thanks to the recent restoration of
some Medicare BBA funds and increases
in provider reimbursement rates in
Michigan’s Medicaid managed care program.
Health Plans Raise Employers’ Premiums
 o cover increased costs and to make
up for losses associated with the insurance
underwriting cycle, Lansing’s two
major health plans-BCBSM and the
Sparrow-sponsored plan, PHP-have
raised employer premiums substantially
in the past two years. Although this is a
national trend, it is especially striking
in Lansing, where premium increases
occurred despite a community-wide
"Save GM" campaign that was trying
to demonstrate to the automobile manufacturer
that Lansing was a good place
to continue to do business-in part
because of the area’s ability to keep
health care costs low. The area’s largest
employers-including GM-were hit
with premium hikes of about 9 percent
in the 1999 contract year and 12 to 15
percent in 2000. Small employers experienced
a wider range of premium increases,
from 10 to 25 percent, with more recent
increases of 20 percent or higher.
While some argue that increased
health plan competition would help
restrain premium increases, this appears
unlikely in Lansing in the foreseeable
future. BCBSM and PHP together account
for the vast majority of the local market
share. The two smaller plans in the Lansing
market (M-Care and Regional Community
Blue) have very small enrollments, perhaps
because they include only one of
Lansing’s two hospital systems (IRMC)
in their networks.
Furthermore, one of the two Lansing
hospitals is said by some respondents to
quote other potential health plan entrants
"unreasonably high" rates for hospital
services, making it extremely difficult for
new plans to enter and compete successfully
in the market. (The hospital maintains
that the higher rates these respondents
quote reflect smaller discounts because of
low volume.) The fact that Lansing has
fewer than 500,000 residents also limits
its attractiveness to large national plans.
Competition has failed to develop in
Lansing’s public sector managed care programs,
as well. The only Medicare managed
care provider is BCBSM’s subsidiary, Blue
Care Network, whose enrollment has
stabilized at about 6,800 members. PHP
decided not to enter Lansing’s Medicare
risk market, concluding that it was unlikely
to be profitable.
The Medicaid managed care market
is dominated by just two plans: PHP
(Sparrow’s affiliated health plan) and
McLaren (IRMC’s affiliated health plan).
A third Medicaid-only health plan (The
Wellness Plan) withdrew from the
Medicaid managed care market in
November 1999, after its contracts with
IRMC and Sparrow were canceled. Two
other Medicaid-only plans (Health Plan
of Michigan and Community Choices)
entered the market anticipating PHP’s
complete withdrawal from the program
but are unlikely to remain because they
have no provider networks and may have
difficulty obtaining one given that both
Sparrow and IRMC have their own
affiliated plans. o cover increased costs and to make
up for losses associated with the insurance
underwriting cycle, Lansing’s two
major health plans-BCBSM and the
Sparrow-sponsored plan, PHP-have
raised employer premiums substantially
in the past two years. Although this is a
national trend, it is especially striking
in Lansing, where premium increases
occurred despite a community-wide
"Save GM" campaign that was trying
to demonstrate to the automobile manufacturer
that Lansing was a good place
to continue to do business-in part
because of the area’s ability to keep
health care costs low. The area’s largest
employers-including GM-were hit
with premium hikes of about 9 percent
in the 1999 contract year and 12 to 15
percent in 2000. Small employers experienced
a wider range of premium increases,
from 10 to 25 percent, with more recent
increases of 20 percent or higher.
While some argue that increased
health plan competition would help
restrain premium increases, this appears
unlikely in Lansing in the foreseeable
future. BCBSM and PHP together account
for the vast majority of the local market
share. The two smaller plans in the Lansing
market (M-Care and Regional Community
Blue) have very small enrollments, perhaps
because they include only one of
Lansing’s two hospital systems (IRMC)
in their networks.
Furthermore, one of the two Lansing
hospitals is said by some respondents to
quote other potential health plan entrants
"unreasonably high" rates for hospital
services, making it extremely difficult for
new plans to enter and compete successfully
in the market. (The hospital maintains
that the higher rates these respondents
quote reflect smaller discounts because of
low volume.) The fact that Lansing has
fewer than 500,000 residents also limits
its attractiveness to large national plans.
Competition has failed to develop in
Lansing’s public sector managed care programs,
as well. The only Medicare managed
care provider is BCBSM’s subsidiary, Blue
Care Network, whose enrollment has
stabilized at about 6,800 members. PHP
decided not to enter Lansing’s Medicare
risk market, concluding that it was unlikely
to be profitable.
The Medicaid managed care market
is dominated by just two plans: PHP
(Sparrow’s affiliated health plan) and
McLaren (IRMC’s affiliated health plan).
A third Medicaid-only health plan (The
Wellness Plan) withdrew from the
Medicaid managed care market in
November 1999, after its contracts with
IRMC and Sparrow were canceled. Two
other Medicaid-only plans (Health Plan
of Michigan and Community Choices)
entered the market anticipating PHP’s
complete withdrawal from the program
but are unlikely to remain because they
have no provider networks and may have
difficulty obtaining one given that both
Sparrow and IRMC have their own
affiliated plans.
Employers Take Modest Steps in Response to Premium Increases
 ansing employers’ responses to premium
increases by health plans have been relatively
modest. The primary strategies used
by employers to limit premium increases
are modifying pharmacy benefits, increasing
cost sharing by employees for some
health maintenance organization (HMO)
services and requiring higher deductibles
in indemnity plans offered to employees.
For the most part, Lansing’s employers
have been absorbing the premium increases.
Several factors may account for this
muted response. First, given the strong
union presence and tight labor market in
Lansing, employees expect relatively comprehensive
health insurance coverage with
limited cost sharing for premiums and broad
choice of providers. About 25 percent of
those with commercial health insurance
coverage in Lansing are enrolled in traditional
indemnity products-a much higher
percentage than the national average. Of
those enrolled in managed care options,
most employees select preferred provider
organizations (PPOs) or point-of-service
(POS) products that offer less restrictive
access to providers than do traditional HMOs.
Second, collective efforts by employers
to reduce cost and monitor quality through
the Capital Area Health Alliance (CAHA)-
a coalition comprising all major stakeholders
in the local health care system-were discontinued
three years ago after the public
release of hospital cost information triggered
providers’ concerns. In the absence
of this information, employers’ collective
efforts to contain costs and improve quality
have been seriously constrained.
Third, Lansing’s three largest
employers-GM, the Michigan state
government and MSU-have adopted
national or statewide purchasing strategies
that shape their view of the Lansing market.
For example, GM views Lansing as a
good place to do business from a health
care benefit standpoint, compared to Flint
and other places where GM plants are
located. GM is also an active member of
the Leapfrog Group, a national coalition of
large employers focusing on improving
patient safety, and reportedly is working
with Lansing hospitals to develop initiatives
to reduce medication errors, a key patient
safety priority identified by Leapfrog.
Statewide needs and concerns similarly
shape the state government’s and university’s
perspectives on health care purchasing
in Lansing.
Finally, the few mid-sized and many
small employers in Lansing have little
clout in negotiations with plans. Given
limited plan options, these employers
typically do not switch health plans in
response to price increases-and even if
they do switch, Lansing’s other plans
apparently do not compete aggressively
for their business. At the same time,
employers have concluded that direct contracting
with providers is unlikely to result
in substantial savings. Small businesses in
Lansing purchase health insurance through
various associations in an effort to improve
their negotiating leverage, but these initiatives
have met with limited success. ansing employers’ responses to premium
increases by health plans have been relatively
modest. The primary strategies used
by employers to limit premium increases
are modifying pharmacy benefits, increasing
cost sharing by employees for some
health maintenance organization (HMO)
services and requiring higher deductibles
in indemnity plans offered to employees.
For the most part, Lansing’s employers
have been absorbing the premium increases.
Several factors may account for this
muted response. First, given the strong
union presence and tight labor market in
Lansing, employees expect relatively comprehensive
health insurance coverage with
limited cost sharing for premiums and broad
choice of providers. About 25 percent of
those with commercial health insurance
coverage in Lansing are enrolled in traditional
indemnity products-a much higher
percentage than the national average. Of
those enrolled in managed care options,
most employees select preferred provider
organizations (PPOs) or point-of-service
(POS) products that offer less restrictive
access to providers than do traditional HMOs.
Second, collective efforts by employers
to reduce cost and monitor quality through
the Capital Area Health Alliance (CAHA)-
a coalition comprising all major stakeholders
in the local health care system-were discontinued
three years ago after the public
release of hospital cost information triggered
providers’ concerns. In the absence
of this information, employers’ collective
efforts to contain costs and improve quality
have been seriously constrained.
Third, Lansing’s three largest
employers-GM, the Michigan state
government and MSU-have adopted
national or statewide purchasing strategies
that shape their view of the Lansing market.
For example, GM views Lansing as a
good place to do business from a health
care benefit standpoint, compared to Flint
and other places where GM plants are
located. GM is also an active member of
the Leapfrog Group, a national coalition of
large employers focusing on improving
patient safety, and reportedly is working
with Lansing hospitals to develop initiatives
to reduce medication errors, a key patient
safety priority identified by Leapfrog.
Statewide needs and concerns similarly
shape the state government’s and university’s
perspectives on health care purchasing
in Lansing.
Finally, the few mid-sized and many
small employers in Lansing have little
clout in negotiations with plans. Given
limited plan options, these employers
typically do not switch health plans in
response to price increases-and even if
they do switch, Lansing’s other plans
apparently do not compete aggressively
for their business. At the same time,
employers have concluded that direct contracting
with providers is unlikely to result
in substantial savings. Small businesses in
Lansing purchase health insurance through
various associations in an effort to improve
their negotiating leverage, but these initiatives
have met with limited success.
Care and Coverage Improves for the Uninsured
 ansing enjoys an uninsurance rate that is
significantly below the national average,
and the Ingham County Health Department
continues to lead collaborative efforts to
improve care and coverage for individuals
without health insurance. In addition to
leading Medicaid and MIChild (the State
Children’s Health Insurance Program)
outreach efforts, the county health department
administers the Ingham Health Plan
(IHP)-a managed care program for
the uninsured.
Under the IHP, the Ingham County
Health Department provides and coordinates
outpatient preventive, primary,
specialty and ancillary care services for
low-income, uninsured adults and
children who are not eligible for public
insurance programs. Already noted for its
success at the time of the previous site
visit, IHP has continued to grow over the
past two years. Currently, it serves approximately
11,500 people-an increase of more
than 50 percent since 1998. Through a new
contract with the MSU faculty practice,
IHP also has expanded access to outpatient
services. A pharmaceutical program created
by IHP in October 2000 obtains volume
discounts of 20 percent on medications
for low-income seniors.
On the horizon are further expansions
of IHP to reach more of the community’s
working poor. Approximately 60 percent
of the program’s current participants are
employed but do not have employer-sponsored
health insurance coverage,
either because their employers do not offer
it or because they cannot afford the premiums.
To reach more of the working poor
who do not have insurance, IHP is planning
to implement a new "third-share"
program in which employers and employees
each contribute one-third of the cost of
premiums, and IHP subsidizes the remaining
one-third. The total premium for
individual coverage is expected to be
approximately $120 per month, making the
monthly cost for individuals roughly $40.
IHP is funded through a combination
of local, state and federal matching
funds-generated by a special Medicaid
disproportionate share hospital (DSH)
payment program-that flow through
IRMC. Despite IRMC’s substantial commitment
to IHP, the special DSH funds
available to the program were limited when
IRMC was the sole hospital participant.
However, after resolving some initial objections,
Sparrow recently decided to participate
in IHP as well, which should bolster
the plan’s funding base and help to support
continued expansion of the number of
people served and providers participating
in the program. New regulations that curtail
the use of federal Medicaid matching
funds for certain services raised concern
about IHP’s continued ability to draw on
DSH funds for support, but state administrators’
interpretation of the ruling is that
the funding stream is secure at this time. ansing enjoys an uninsurance rate that is
significantly below the national average,
and the Ingham County Health Department
continues to lead collaborative efforts to
improve care and coverage for individuals
without health insurance. In addition to
leading Medicaid and MIChild (the State
Children’s Health Insurance Program)
outreach efforts, the county health department
administers the Ingham Health Plan
(IHP)-a managed care program for
the uninsured.
Under the IHP, the Ingham County
Health Department provides and coordinates
outpatient preventive, primary,
specialty and ancillary care services for
low-income, uninsured adults and
children who are not eligible for public
insurance programs. Already noted for its
success at the time of the previous site
visit, IHP has continued to grow over the
past two years. Currently, it serves approximately
11,500 people-an increase of more
than 50 percent since 1998. Through a new
contract with the MSU faculty practice,
IHP also has expanded access to outpatient
services. A pharmaceutical program created
by IHP in October 2000 obtains volume
discounts of 20 percent on medications
for low-income seniors.
On the horizon are further expansions
of IHP to reach more of the community’s
working poor. Approximately 60 percent
of the program’s current participants are
employed but do not have employer-sponsored
health insurance coverage,
either because their employers do not offer
it or because they cannot afford the premiums.
To reach more of the working poor
who do not have insurance, IHP is planning
to implement a new "third-share"
program in which employers and employees
each contribute one-third of the cost of
premiums, and IHP subsidizes the remaining
one-third. The total premium for
individual coverage is expected to be
approximately $120 per month, making the
monthly cost for individuals roughly $40.
IHP is funded through a combination
of local, state and federal matching
funds-generated by a special Medicaid
disproportionate share hospital (DSH)
payment program-that flow through
IRMC. Despite IRMC’s substantial commitment
to IHP, the special DSH funds
available to the program were limited when
IRMC was the sole hospital participant.
However, after resolving some initial objections,
Sparrow recently decided to participate
in IHP as well, which should bolster
the plan’s funding base and help to support
continued expansion of the number of
people served and providers participating
in the program. New regulations that curtail
the use of federal Medicaid matching
funds for certain services raised concern
about IHP’s continued ability to draw on
DSH funds for support, but state administrators’
interpretation of the ruling is that
the funding stream is secure at this time.
Issues to Track
 ising premiums, limited plan competition
and increased service competition
observed over the last two years suggest
that controlling health care costs may prove
very difficult for Lansing employers in the
future. Consequently, employees and their
unions may face difficult choices about
health care coverage and benefits. In addition,
state regulators may increasingly face
complex questions about provider capacity
and competition among plans, hospitals
and physicians. As the Lansing market
continues to evolve, it will be important
to track the following questions: ising premiums, limited plan competition
and increased service competition
observed over the last two years suggest
that controlling health care costs may prove
very difficult for Lansing employers in the
future. Consequently, employees and their
unions may face difficult choices about
health care coverage and benefits. In addition,
state regulators may increasingly face
complex questions about provider capacity
and competition among plans, hospitals
and physicians. As the Lansing market
continues to evolve, it will be important
to track the following questions:
- Will hospitals continue to be able to
sustain higher payment rates from
health plans?
- What impact will increased competition
among hospitals and physician
entrepreneurs for select clinical services
have on costs, quality and access to care?
- How will employers respond to rising
premiums, particularly if the economy
slows? What leverage can employers
exert in a highly consolidated market
with a heavily unionized workforce that
expects comprehensive coverage and
provider choice?
- Will the Ingham County Health Department’s planned expansions succeed, and
what impact will they have on coverage and care for the uninsured?
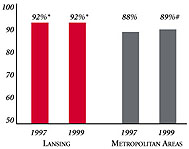
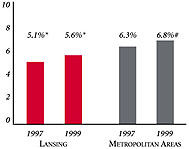
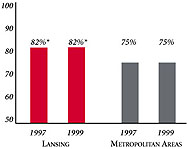
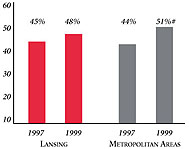
Lansing’s Experience with the Local Health System, 1997 and
1999
Background and Observations
| Lansing Demographics |
| Lansing |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
450,789 |
| Population Change, 1990-19992
|
| 4.2% |
8.6% |
| Median Income3 |
| $30,830 |
$27,843 |
| Persons Living in Poverty3 |
| 11% |
14% |
| Persons Age 65 or Older3 |
| 10% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Lansing |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 8.2% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 4.0% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 85% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $183 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Lansing |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 2.2 |
2.8 |
| Physicians per 1,000 Population2
|
| 2.1 |
2.3 |
| HMO Penetration, 19973 |
| 41% |
32% |
| HMO Penetration, 19994 |
| 41% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Lansing Community Report:
Kelly Devers, HSC
Jon B. Christianson, University of Minnesota
Laurie E. Felland, HSC
Sue Felt-Lisk, Mathematica Policy Research, Inc.
Liza Rudell, HSC
J. Lee Hargraves, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|