Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Insurance Coverage & Costs
Access to Care
Quality & Care Delivery
Health Care Markets
Employers/Consumers
Health Plans
Hospitals
Physicians
Issue Briefs
Data Bulletins
Research Briefs
Policy Analyses
Community Reports
Journal Articles
Other Publications
Surveys
Site Visits
Design and Methods
Data Files
|


HMO Model Shaken but Remains Intact
Orange County, Calif.
Community Report No. 09
Summer 2001
Aaron Katz, Robert E. Hurley, Leslie A. Jackson, Timothy K. Lake, Ashley C. Short, Paul B. Ginsburg, Joy M. Grossman
 n January 2001, a team of researchers
visited Orange County, Calif., to study
that community’s health system, how
it is changing and the effects of those
changes on consumers. The Center for
Studying Health System Change
(HSC), as part of the Community
Tracking Study, interviewed more
than 80 leaders in the health care market.
Orange County is one of 12
communities tracked by HSC every
two years through site visits and surveys.
Individual community reports
are published for each round of site
visits. The first two site visits to Orange
County, in 1996 and 1998, provided
baseline and initial trend information
against which changes are tracked.
The Orange County market encompasses
an area of about 30 cities south
of Los Angeles. n January 2001, a team of researchers
visited Orange County, Calif., to study
that community’s health system, how
it is changing and the effects of those
changes on consumers. The Center for
Studying Health System Change
(HSC), as part of the Community
Tracking Study, interviewed more
than 80 leaders in the health care market.
Orange County is one of 12
communities tracked by HSC every
two years through site visits and surveys.
Individual community reports
are published for each round of site
visits. The first two site visits to Orange
County, in 1996 and 1998, provided
baseline and initial trend information
against which changes are tracked.
The Orange County market encompasses
an area of about 30 cities south
of Los Angeles.
Despite sustained turmoil in the Orange County health care market, health maintenance
organizations (HMOs) continue to dominate. The market remains unique, not only
because of extensive enrollment in HMOs, but also because large physician organizations
assume much of the financial risk and care management that is typically within
health plans’ purview. Plans, providers and consumers have been comfortable with
this arrangement, so Orange County has not yet seen the shift from HMOs to preferred
provider organizations (PPOs) experienced elsewhere.
Nevertheless, turmoil among physician organizations
shook the market two years ago, and several recent
developments continue to threaten its stability:
- The market’s largest physician practice management
company (PPMC) declared bankruptcy, jeopardizing
access and quality for patients.
- A premier hospital system, along with affiliated
physicians, terminated its contract with the market’s
leading health plan, disrupting access to care.
-
The market is bracing for a rapid rise in its historically low HMO premiums, which
may result in higher consumer cost sharing and expansion of PPOs.
Unstable Provider Networks Provoke Concerns
 ince 1998, two major disruptions have
shaken and destabilized provider networks
in Orange County. The first was
the bankruptcy in November 2000
of KPC Medical Management, the area’s
largest PPMC. The second was a decision
by the largest provider, St. Joseph Health
System, to drop several HMO contracts,
including its contract with PacifiCare, one
of the county’s leading longtime health
plans. These disruptions have heightened
concerns among consumers, health
plans and employers and increased regulatory
scrutiny.
KPC’s Demise. KPC’s abrupt closure of 38 clinics and the subsequent bankruptcy
temporarily disrupted access to medical care for up to 300,000 people. Furthermore,
KPC’s failure to transmit patient records and test results in a timely manner-attributed
to the group’s financial distress-raised concerns about quality of care.
The demise of KPC signaled the end
of the PPMC model in Orange County.
PPMCs were designed to organize large
numbers of physicians into networks to
accept financial risk, streamline practice
management and negotiate with health
plans. Once expected to flourish in Orange
County, PPMCs have struggled since 1998.
Two forerunners to KPC-MedPartners
and FPA, Inc.-failed in 1998, disrupting
patient care in the county and raising questions
about the state’s role in overseeing
capitated payment arrangements between
provider organizations and health plans.
KPC’s financial difficulties ignited a
political and public relations battle between
state medical and health plan associations,
and California policy makers took several
steps to intervene. Gov. Gray Davis’
administration encouraged several health
plans to contribute to a financial assistance
package to keep KPC operating. Although
a $30 million loan package was negotiated,
KPC failed nonetheless. After KPC filed
for bankruptcy protection, a judge installed
a new director of the organization to ensure
that medical records were distributed to
patients’ new providers as quickly as possible
to avoid the protracted problems
that occurred two years ago.
The newly created state Department
of Managed Health Care also stepped in
to ensure access to care by working with
health plans to facilitate the transfer of
KPC patients to other providers. The
agency was not able to be more proactive
because KPC’s operating status was not
within the purview of California regulators.
Newly issued rules requiring physician
organizations to report financial data are
intended to improve oversight and to
avoid future problems.
St. Joseph and PacifiCare Part Ways. In a bold move, St. Joseph Health
System announced in June 2000 that it would terminate all 14 of its existing HMO
contracts and, through a competitive bidding process, select five plans with which
it would establish five-year contracts. The system’s decision to terminate its
contract with PacifiCare, which St. Joseph says will stand for at least five years,
ended a long-standing relationship between the two organizations. About half of
the 100,000 PacifiCare members in Orange County who received care at St. Joseph
may change insurers so they can remain with their St. Joseph provider when the
current contract ends in July 2001.
Consumer Concerns Grow. KPC’s bankruptcy and St. Joseph’s contract termination
have increased concerns among health plans and purchasers that provider network
instability will jeopardize access, continuity of care and customer service. Some
health plans, such as Blue Shield and CIGNA, have tried to pull members out of
failing physician organizations to avert access and quality problems. To prevent
organizational failures and improve physician organizations’ overall financial
and clinical performance, nearly all plans have devised surveillance and consultation
strategies.
Employers are concerned that employees
will have a diminishing choice of providers.
Some employers dropped PacifiCare when
St. Joseph terminated its contract, but others
have taken a wait-and-see approach.
Because the St. Joseph/PacifiCare break
occurred after many employers had made
their 2001 plan offerings, its full effect on
employees may not be seen until next year. ince 1998, two major disruptions have
shaken and destabilized provider networks
in Orange County. The first was
the bankruptcy in November 2000
of KPC Medical Management, the area’s
largest PPMC. The second was a decision
by the largest provider, St. Joseph Health
System, to drop several HMO contracts,
including its contract with PacifiCare, one
of the county’s leading longtime health
plans. These disruptions have heightened
concerns among consumers, health
plans and employers and increased regulatory
scrutiny.
KPC’s Demise. KPC’s abrupt closure of 38 clinics and the subsequent bankruptcy
temporarily disrupted access to medical care for up to 300,000 people. Furthermore,
KPC’s failure to transmit patient records and test results in a timely manner-attributed
to the group’s financial distress-raised concerns about quality of care.
The demise of KPC signaled the end
of the PPMC model in Orange County.
PPMCs were designed to organize large
numbers of physicians into networks to
accept financial risk, streamline practice
management and negotiate with health
plans. Once expected to flourish in Orange
County, PPMCs have struggled since 1998.
Two forerunners to KPC-MedPartners
and FPA, Inc.-failed in 1998, disrupting
patient care in the county and raising questions
about the state’s role in overseeing
capitated payment arrangements between
provider organizations and health plans.
KPC’s financial difficulties ignited a
political and public relations battle between
state medical and health plan associations,
and California policy makers took several
steps to intervene. Gov. Gray Davis’
administration encouraged several health
plans to contribute to a financial assistance
package to keep KPC operating. Although
a $30 million loan package was negotiated,
KPC failed nonetheless. After KPC filed
for bankruptcy protection, a judge installed
a new director of the organization to ensure
that medical records were distributed to
patients’ new providers as quickly as possible
to avoid the protracted problems
that occurred two years ago.
The newly created state Department
of Managed Health Care also stepped in
to ensure access to care by working with
health plans to facilitate the transfer of
KPC patients to other providers. The
agency was not able to be more proactive
because KPC’s operating status was not
within the purview of California regulators.
Newly issued rules requiring physician
organizations to report financial data are
intended to improve oversight and to
avoid future problems.
St. Joseph and PacifiCare Part Ways. In a bold move, St. Joseph Health
System announced in June 2000 that it would terminate all 14 of its existing HMO
contracts and, through a competitive bidding process, select five plans with which
it would establish five-year contracts. The system’s decision to terminate its
contract with PacifiCare, which St. Joseph says will stand for at least five years,
ended a long-standing relationship between the two organizations. About half of
the 100,000 PacifiCare members in Orange County who received care at St. Joseph
may change insurers so they can remain with their St. Joseph provider when the
current contract ends in July 2001.
Consumer Concerns Grow. KPC’s bankruptcy and St. Joseph’s contract termination
have increased concerns among health plans and purchasers that provider network
instability will jeopardize access, continuity of care and customer service. Some
health plans, such as Blue Shield and CIGNA, have tried to pull members out of
failing physician organizations to avert access and quality problems. To prevent
organizational failures and improve physician organizations’ overall financial
and clinical performance, nearly all plans have devised surveillance and consultation
strategies.
Employers are concerned that employees
will have a diminishing choice of providers.
Some employers dropped PacifiCare when
St. Joseph terminated its contract, but others
have taken a wait-and-see approach.
Because the St. Joseph/PacifiCare break
occurred after many employers had made
their 2001 plan offerings, its full effect on
employees may not be seen until next year.
Back to Top
Capitated, Delegated Managed
Care Survives—for Now
 anaged care has long been widespread
and aggressive in Orange County. HMO
penetration hovers around 50 percent,
and health plans continue to delegate
considerable financial risk to providers-
including not only physicians’ fees, but
also ancillary services and sometimes
hospital care. The recent provider network
instability and continued turmoil
among physician organizations are a sign,
however, that big changes may be on
the horizon.
Hospitals in Orange County, like their
counterparts nationally, have experienced
financial hardship from reductions in
Medicare revenue under the 1997 Balanced
Budget Act and rising costs. In addition,
many Orange County and other California
hospitals must renovate facilities to comply
with state seismic standards, an
undertaking that could require as much
as $24 billion in hospital capital spending
statewide (reportedly more than the total
value of existing facilities) by 2030.
Moreover, labor shortages, which have
been driving up costs nationally, have
been particularly severe in Orange County,
where as many as 20 percent of hospital
nursing positions are vacant.
In response to such pressures, many
hospitals are refusing to accept capitated
payment for their services. Tenet Healthcare
Corp., which operates 10 hospitals in the
county, and the University of California-
Irvine Medical Center have decided to
drop capitation payment as their HMO
contracts come up for renewal. Similarly,
St. Joseph has eliminated hospital capitation
in newly negotiated contracts.
Meanwhile, physician organizations-
which typically bear the lion’s share of
financial risk in the Orange County market-
have continued to struggle under
capitation rates that they contend have
not kept pace with rising costs. Many are
now trying to shed risk for ancillary services
such as pharmacy or injectable
drugs, which they view as too difficult
and unpredictable to manage. Physician
organizations are retaining risk for professional
services but pushing for higher
capitation rates to cover costs.
Market observers worry that providers’
dramatic pushback on risk contracting
and demand for higher payments eventually
may undermine the substantial price
advantage HMOs have enjoyed in the
county and open the market to growth
of more expensive and less aggressively
managed products, such as PPOs. In fact,
driven by fears of more provider network
instability and already rising premiums,
health plans are positioning themselves
for a possible shift toward PPOs by
preparing for fee-for-service contracts
with individual physicians.
Any shift away from HMOs in Orange
County is still down the road, because
many physician organizations and health
plans in the market remain firmly committed
to the fully delegated model of
capitated managed care. Indeed, large
barriers stand in the way of such a shift:
Physician organizations would have to
greatly expand their ability to bill for
services, and health plans would have to
develop the capacity to manage service
utilization now handled by physician
practices. anaged care has long been widespread
and aggressive in Orange County. HMO
penetration hovers around 50 percent,
and health plans continue to delegate
considerable financial risk to providers-
including not only physicians’ fees, but
also ancillary services and sometimes
hospital care. The recent provider network
instability and continued turmoil
among physician organizations are a sign,
however, that big changes may be on
the horizon.
Hospitals in Orange County, like their
counterparts nationally, have experienced
financial hardship from reductions in
Medicare revenue under the 1997 Balanced
Budget Act and rising costs. In addition,
many Orange County and other California
hospitals must renovate facilities to comply
with state seismic standards, an
undertaking that could require as much
as $24 billion in hospital capital spending
statewide (reportedly more than the total
value of existing facilities) by 2030.
Moreover, labor shortages, which have
been driving up costs nationally, have
been particularly severe in Orange County,
where as many as 20 percent of hospital
nursing positions are vacant.
In response to such pressures, many
hospitals are refusing to accept capitated
payment for their services. Tenet Healthcare
Corp., which operates 10 hospitals in the
county, and the University of California-
Irvine Medical Center have decided to
drop capitation payment as their HMO
contracts come up for renewal. Similarly,
St. Joseph has eliminated hospital capitation
in newly negotiated contracts.
Meanwhile, physician organizations-
which typically bear the lion’s share of
financial risk in the Orange County market-
have continued to struggle under
capitation rates that they contend have
not kept pace with rising costs. Many are
now trying to shed risk for ancillary services
such as pharmacy or injectable
drugs, which they view as too difficult
and unpredictable to manage. Physician
organizations are retaining risk for professional
services but pushing for higher
capitation rates to cover costs.
Market observers worry that providers’
dramatic pushback on risk contracting
and demand for higher payments eventually
may undermine the substantial price
advantage HMOs have enjoyed in the
county and open the market to growth
of more expensive and less aggressively
managed products, such as PPOs. In fact,
driven by fears of more provider network
instability and already rising premiums,
health plans are positioning themselves
for a possible shift toward PPOs by
preparing for fee-for-service contracts
with individual physicians.
Any shift away from HMOs in Orange
County is still down the road, because
many physician organizations and health
plans in the market remain firmly committed
to the fully delegated model of
capitated managed care. Indeed, large
barriers stand in the way of such a shift:
Physician organizations would have to
greatly expand their ability to bill for
services, and health plans would have to
develop the capacity to manage service
utilization now handled by physician
practices.
Back to Top
Providers Redirect Market Strategies
 n the late 1990s, provider efforts in Orange County and elsewhere
emphasized integrating inpatient and outpatient services, thereby creating networks
or systems that could take risk for and coordinate the whole range of medical
care. The failure of risk-bearing intermediaries and growing pressures on revenues
and capacity-from population increases, labor shortages and low payment rates-have
led to a shift away from integration strategies among both hospitals and physicians.
Hospitals Build, Specialize. As Orange County hospitals move away from
capitated payment arrangements, they increasingly have focused on building revenue-
generating services. This strategy is motivated in part by changed financial incentives
and in part by newly emerging capacity problems. After trying to reduce excess
capacity for years, many prominent hospitals apparently now face capacity constraints.
Hospitals attribute this change to labor shortages, growing demand for services
and, thanks to more accommodating HMO products, greater consumer leeway in choosing
providers.
Hospitals have responded by turning
their attention to building inpatient and
outpatient capacity, improving their brand
identities in both geographic and product
markets and developing specialty-focused,
centers of excellence. For example: n the late 1990s, provider efforts in Orange County and elsewhere
emphasized integrating inpatient and outpatient services, thereby creating networks
or systems that could take risk for and coordinate the whole range of medical
care. The failure of risk-bearing intermediaries and growing pressures on revenues
and capacity-from population increases, labor shortages and low payment rates-have
led to a shift away from integration strategies among both hospitals and physicians.
Hospitals Build, Specialize. As Orange County hospitals move away from
capitated payment arrangements, they increasingly have focused on building revenue-
generating services. This strategy is motivated in part by changed financial incentives
and in part by newly emerging capacity problems. After trying to reduce excess
capacity for years, many prominent hospitals apparently now face capacity constraints.
Hospitals attribute this change to labor shortages, growing demand for services
and, thanks to more accommodating HMO products, greater consumer leeway in choosing
providers.
Hospitals have responded by turning
their attention to building inpatient and
outpatient capacity, improving their brand
identities in both geographic and product
markets and developing specialty-focused,
centers of excellence. For example:
- Hoag Memorial is planning to build a new
patient tower with an obstetrics/gynecology
focus and outpatient cardiology and
oncology facilities.
- Similarly, St. Joseph Hospital is building a new patient care tower and new
cardiology and oncology outpatient units in partnership with specialty physicians.
- MemorialCare, which has increased its capacity by buying two hospitals, is
striving to establish its identity as the county’s premier, high-quality hospital
system.
Physician Organizations Largely Intact. The physician market in Orange
County remains highly organized, despite KPC’s demise. Large primary care or multispecialty
physician groups and independent practice associations (IPAs) -some of which were
part of KPC- continue to dominate the county’s landscape and wield considerable
clout with health plans.
For example, Monarch Healthcare IPA, the largest independent physician organization
in the market, contracts with 800 physicians, including 250 primary care physicians,
most of whom practice in small groups or solo practices. Monarch serves about
150,000 HMO enrollees, including 20,000 Medicare+Choice enrollees. The IPA has
substantial negotiating leverage with health plans and strong leverage over local
physicians practicing in southern Orange County.
Damage from the MedPartners/KPC downfall and historically low fees continue to
affect physician practices, and many of the preexisting groups have shrunk. Most
of the physician organizations that were acquired by MedPartners have become independent
again, but many physicians in these organizations have moved to smaller practices.
Moreover, physician organizations are widely perceived to be in worse financial
condition as a result of years of inadequate investment and the need for more
working capital than usual because of late payments from plans.
Back to Top
Plans See Enrollment Shifts,
Employers Face Premium Hikes
 lthough the number of major health plans in Orange County
has changed little in the past two years, turbulence in provider contracts and
impending health plan premium increases have created instability and uncertainty
in the health plan market (see box). Indeed, by March 2001,
PacifiCare’s large Medicare product, Secure Horizons, had already lost 10,000
members in Orange County. Adding to PacifiCare’s woes nationally were leadership
turnover, strict federal caps on Medicare payment increases and a sharp drop in
its stock price.
Recent federal limits on payment increases for Medicare managed care plans also
are a cause of concern. Though the Medicare+Choice market in Orange County is
still attractive to health plans and beneficiaries-42 percent are in HMOs-plans
are trimming benefits and putting enrollees on notice for more changes down the
line. PacifiCare, whose Secure Horizons is the nation’s largest Medicare HMO and
covers more than 60,000 enrollees in Orange County, reduced its prescription drug
benefit, and Kaiser added a $20 monthly premium for its 23,000 Medicare beneficiaries.
Observers expect these types of changes to increase enrollment shifts among major
health plans in the local Medicare market.
More turmoil is expected in the
county’s commercial market as employers
brace for double-digit premium increases
from health plans. Some employers are
trying to hold down cost increases in the
short term through benefit modifications,
such as increasing consumer copayments
and deductibles and instituting three-tiered
pharmacy benefits. For example, the
California Public Employees’ Retirement
System (CalPERS)-viewed as a bellwether
for employer benefit strategies locally and
nationally-responded to proposed double-digit
premium increases for its fully insured
HMO products in 2002 by rejecting all
HMO contracts and requesting new bids.
This tactic, along with increased copay-ments
for office visits and prescription
drugs, allowed CalPERS to hold its HMO
premium increases to 6 percent.
Employers worry that the higher payment rates obtained by St. Joseph and other
providers, along with increased utilization rates and prescription drugs costs,
will push premiums up even faster over the next few years. Meanwhile, dissatisfaction
with the quality of customer service by carriers is rising among both employers
and employees, adding impetus for a potential move away from HMOs in favor of
more loosely managed products such as PPOs. lthough the number of major health plans in Orange County
has changed little in the past two years, turbulence in provider contracts and
impending health plan premium increases have created instability and uncertainty
in the health plan market (see box). Indeed, by March 2001,
PacifiCare’s large Medicare product, Secure Horizons, had already lost 10,000
members in Orange County. Adding to PacifiCare’s woes nationally were leadership
turnover, strict federal caps on Medicare payment increases and a sharp drop in
its stock price.
Recent federal limits on payment increases for Medicare managed care plans also
are a cause of concern. Though the Medicare+Choice market in Orange County is
still attractive to health plans and beneficiaries-42 percent are in HMOs-plans
are trimming benefits and putting enrollees on notice for more changes down the
line. PacifiCare, whose Secure Horizons is the nation’s largest Medicare HMO and
covers more than 60,000 enrollees in Orange County, reduced its prescription drug
benefit, and Kaiser added a $20 monthly premium for its 23,000 Medicare beneficiaries.
Observers expect these types of changes to increase enrollment shifts among major
health plans in the local Medicare market.
More turmoil is expected in the
county’s commercial market as employers
brace for double-digit premium increases
from health plans. Some employers are
trying to hold down cost increases in the
short term through benefit modifications,
such as increasing consumer copayments
and deductibles and instituting three-tiered
pharmacy benefits. For example, the
California Public Employees’ Retirement
System (CalPERS)-viewed as a bellwether
for employer benefit strategies locally and
nationally-responded to proposed double-digit
premium increases for its fully insured
HMO products in 2002 by rejecting all
HMO contracts and requesting new bids.
This tactic, along with increased copay-ments
for office visits and prescription
drugs, allowed CalPERS to hold its HMO
premium increases to 6 percent.
Employers worry that the higher payment rates obtained by St. Joseph and other
providers, along with increased utilization rates and prescription drugs costs,
will push premiums up even faster over the next few years. Meanwhile, dissatisfaction
with the quality of customer service by carriers is rising among both employers
and employees, adding impetus for a potential move away from HMOs in favor of
more loosely managed products such as PPOs.
Back to Top
Tobacco Money Galvanizes
Safety Net
 range County’s fragile safety net system
appears to be getting stronger and more
organized. Many are optimistic that the
state’s new tobacco-related funds, along
with existing and expanding public insurance
programs, will help improve the overall
capacity of both community clinics and
major safety net hospitals. On the other
hand, local political conflicts, potential state
and federal program budget constraints and
a possible economic downturn could threaten
the well-being of safety net providers and
uninsured families alike.
Funds from the new state tobacco
tax and the state’s tobacco settlement
promise important gains for the local
safety net. Orange County has set aside
part of its $50 million allocation from the
state tobacco tax to develop comprehensive
health and early childhood development
programs for children under 6. This
money will help to expand access at the
region’s two major safety net hospitals,
Children’s Hospital of Orange County
and University of California-Irvine Medical
Center. The state also plans to allocate $24
million a year in tobacco settlement funds
to health services that will benefit safety
net providers as well. Community clinics
in Orange County, for example, will receive
about $3.5 million for expansions.
In addition, the State Children’s
Health Insurance Program (SCHIP),
Healthy Families, has expanded coverage
to about one-third of the county’s estimated
90,000 uninsured children, thanks
largely to targeted outreach efforts by
community organizations. A recent
expansion of eligibility for children and a
newly submitted federal waiver to expand
Healthy Families to the parents of eligible
children are expected to help even more.
CalOPTIMA, a quasi-public agency that
oversees the county’s Medicaid managed
care program, has been instrumental in
the success of Healthy Families-and the
continued strength of the safety net-in
coordinating outreach and new strategies
to address the uninsured.
Despite these improvements, the safety
net and uninsured families in Orange County
remain vulnerable. First and foremost, many
observers fear that if the economy worsens,
uninsurance will grow beyond the already
high rate of one in five people. The rising
number of non-English-speaking immigrants
presents an added challenge to the
local safety net. Many advocates worry
that the county’s limited medically indigent
program leaves many needy people without
care and, because of its low payment
levels, increases the charity care burden
on providers. And while advocates are
buoyed by expanded public programs
and funding, they worry that tobacco
revenues will dry up and that federal or
state budget decisions-perhaps as fallout
from the state’s energy crisis-will jeopardize
recent coverage expansions. range County’s fragile safety net system
appears to be getting stronger and more
organized. Many are optimistic that the
state’s new tobacco-related funds, along
with existing and expanding public insurance
programs, will help improve the overall
capacity of both community clinics and
major safety net hospitals. On the other
hand, local political conflicts, potential state
and federal program budget constraints and
a possible economic downturn could threaten
the well-being of safety net providers and
uninsured families alike.
Funds from the new state tobacco
tax and the state’s tobacco settlement
promise important gains for the local
safety net. Orange County has set aside
part of its $50 million allocation from the
state tobacco tax to develop comprehensive
health and early childhood development
programs for children under 6. This
money will help to expand access at the
region’s two major safety net hospitals,
Children’s Hospital of Orange County
and University of California-Irvine Medical
Center. The state also plans to allocate $24
million a year in tobacco settlement funds
to health services that will benefit safety
net providers as well. Community clinics
in Orange County, for example, will receive
about $3.5 million for expansions.
In addition, the State Children’s
Health Insurance Program (SCHIP),
Healthy Families, has expanded coverage
to about one-third of the county’s estimated
90,000 uninsured children, thanks
largely to targeted outreach efforts by
community organizations. A recent
expansion of eligibility for children and a
newly submitted federal waiver to expand
Healthy Families to the parents of eligible
children are expected to help even more.
CalOPTIMA, a quasi-public agency that
oversees the county’s Medicaid managed
care program, has been instrumental in
the success of Healthy Families-and the
continued strength of the safety net-in
coordinating outreach and new strategies
to address the uninsured.
Despite these improvements, the safety
net and uninsured families in Orange County
remain vulnerable. First and foremost, many
observers fear that if the economy worsens,
uninsurance will grow beyond the already
high rate of one in five people. The rising
number of non-English-speaking immigrants
presents an added challenge to the
local safety net. Many advocates worry
that the county’s limited medically indigent
program leaves many needy people without
care and, because of its low payment
levels, increases the charity care burden
on providers. And while advocates are
buoyed by expanded public programs
and funding, they worry that tobacco
revenues will dry up and that federal or
state budget decisions-perhaps as fallout
from the state’s energy crisis-will jeopardize
recent coverage expansions.
Back to Top
Issues to Track
 he Orange County health market is a place of contrasts. All
players-providers, insurers, purchasers and consumers- continue to rely on HMO
products and delegated risk and care management. In addition, managed care is
highly successful and stable in the Medicare, Medicaid and SCHIP programs. But
the ongoing turmoil in physician organizations and in provider-health plan relations
may lead to dramatic changes. As the market continues to unfold, the following
issues will be important to track: he Orange County health market is a place of contrasts. All
players-providers, insurers, purchasers and consumers- continue to rely on HMO
products and delegated risk and care management. In addition, managed care is
highly successful and stable in the Medicare, Medicaid and SCHIP programs. But
the ongoing turmoil in physician organizations and in provider-health plan relations
may lead to dramatic changes. As the market continues to unfold, the following
issues will be important to track:
- Will increasing provider payment and
scrutiny of physician organization finances
help to stabilize the provider market? If
so, how will health plan premiums and
consumer access to care be affected?
- Will purchasers respond to rising premiums by reducing benefits or shifting
costs to consumers?
- To what extent will PPOs and other less restricted network products emerge,
and how will they be received by purchasers, consumers and providers long
accustomed to HMOs?
- Will collaborations involving new tobacco-related
funding be sustained and result
in stronger and more widely accessible
safety net services?
Back to Top
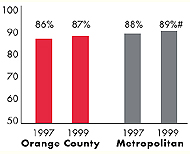
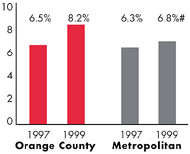
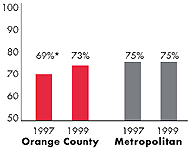
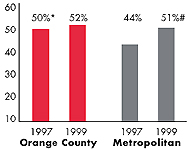
Orange County’s Experience with the Local Health System, 1997
and 1999
Back to Top
Background and Observations
| Orange County Demographics |
| Orange County |
Metropolitan areas above 200,000 population |
Population, July 1, 19991
2,760,948 |
| Population Change, 1990-19992
|
| 15% |
8.6% |
| Median Income3 |
| $30,635 |
$27,843 |
| Persons Living in Poverty3 |
| 11% |
14% |
| Persons Age 65 or Older3 |
| 11% |
11% |
Sources:
1. US Bureau of Census, 1999 Community Population Estimates
2. US Bureau of Census, 1990 & 1999 Community Population Estimates
3. Community Tracking Study Household Survey, 1998-1999 |
| Health Insurance Status |
| Orange County |
Metropolitan areas above 200,000 population |
| Persons under Age 65 with No Health Insurance1 |
| 18% |
15% |
| Children under Age 18 with No Health Insurance1
|
| 15% |
11% |
| Employees Working for Private Firms that
Offer Coverage2 |
| 81% |
84% |
| Average Monthly Premium for Self-Only Coverage
under Employer-Sponsored Insurance2 |
| $156 |
$181 |
Sources:
1. Community Tracking Study Household Survey, 1998-1999
2. Robert Wood Johnson Foundation Employer Health Insurance Survey, 1997 |
| Health System Characteristics |
| Orange County |
Metropolitan areas above 200,000 population |
| Staffed Hospital Beds per 1,000 Population1
|
| 2.1 |
2.8 |
| Physicians per 1,000 Population2
|
| 2.2 |
2.3 |
| HMO Penetration, 19973 |
| 46% |
32% |
| HMO Penetration, 19994 |
| 46% |
36% |
Sources:
1. American Hospital Association, 1998
2. Area Resource File, 1998 (includes nonfederal, patient care physicians,
except radiologists, pathologists and anesthesiologists)
3. InterStudy Competitive Edge 8.1
4. InterStudy Competitive Edge 10.1 |
Back to Top
Instability and Uncertainty among Health Plans: Who Benefits?
 ith PacifiCare under duress, the pole position among Orange County health
plans appears to be shifting to Kaiser, which has grown steadily over the past five
years to more than 300,000 enrollees. Kaiser has bounced back from the financial
stress and capacity problems that were evident in 1998. Furthermore, it has
escaped—and, indeed, benefited from—provider network stability issues because
of its group-model structure built around an exclusive relationship with a single
large medical group and affiliated hospitals. Kaiser reportedly is ahead of its competitors
in its use of disease management initiatives and Web-based communications
with consumers, in part because members stay with the health plan for an average
of 12 years.
Other health plans may benefit from shifts and uncertainty in Orange County’s
health insurance market. Some health plans that already offer PPOs—such as
Wellpoint’s Blue Cross of California, Blue Shield of California, CIGNA and Aetna—
may be more agile in the changing health plan market. These plans have developed
individual, nonrisk contracts with physicians under PPOs, as well as utilization
management programs, that would allow them to grow if and when the market
shifts away from HMOs. PPOs may be less susceptible to large-scale disruptions
from provider pushback because they rely on individual contracts with physicians. ith PacifiCare under duress, the pole position among Orange County health
plans appears to be shifting to Kaiser, which has grown steadily over the past five
years to more than 300,000 enrollees. Kaiser has bounced back from the financial
stress and capacity problems that were evident in 1998. Furthermore, it has
escaped—and, indeed, benefited from—provider network stability issues because
of its group-model structure built around an exclusive relationship with a single
large medical group and affiliated hospitals. Kaiser reportedly is ahead of its competitors
in its use of disease management initiatives and Web-based communications
with consumers, in part because members stay with the health plan for an average
of 12 years.
Other health plans may benefit from shifts and uncertainty in Orange County’s
health insurance market. Some health plans that already offer PPOs—such as
Wellpoint’s Blue Cross of California, Blue Shield of California, CIGNA and Aetna—
may be more agile in the changing health plan market. These plans have developed
individual, nonrisk contracts with physicians under PPOs, as well as utilization
management programs, that would allow them to grow if and when the market
shifts away from HMOs. PPOs may be less susceptible to large-scale disruptions
from provider pushback because they rely on individual contracts with physicians.
Back to Top

The Community Tracking Study, the major effort of the Center for Studying Health
System Change (HSC), tracks changes in the health system in 60 sites that are
representative of the nation. Every two years, HSC conducts surveys in all 60
communities and site visits in 12 communities. The Community Report series documents
the findings from the third round of site visits. Analyses based on site visit
and survey data from the Community Tracking Study are published by HSC in Issue
Briefs, Data Bulletins and peer-reviewed journals. These publications are
available at www.hschange.org.
Authors of the Orange County Community Report:
Aaron Katz, University
of Washington
Robert E. Hurley, Virginia Commonwealth University
Leslie Jackson,
HSC
Timothy K. Lake, Mathematica Policy Research, Inc.
Ashley C. Short, HSC
Paul B. Ginsburg, HSC
Joy M. Grossman, HSC
Community Reports are published by HSC:
President: Paul B. Ginsburg
Director of Site Visits: Cara S. Lesser
Director of Public Affairs: Ann C. Greiner
Editor: The Stein Group
|